Two OUWB officials have recently tried to do something about it because no one in healthcare is immune to calling burnout a “silent pandemic.”
“Burnout in Health Care: Causes, Consequences, and Coping Strategies” was recently published by Changiz Mohiyeddini Ph.D., professor of the Department of Foundational Medical Studies and Associate Dean of Clinical Education, Pierre Morris, MD. The workshop was organized by the OUWB Center for Excellence Medical Education.
The hope was to raise awareness of the problem, promote a better understanding of the causes and mechanisms of burnout, and provide tips to avoid it.
“Medical students, doctors, nurses… (burnout) affects all healthcare,” Mohiyeddini said.
The two relied on Medscape's doctor Burnout & Depression Report 2024 to shed light on the range of issues. The report was prepared after 9,226 people responded to the survey between July 5th and October 9th, 2023.
Morris (left) and Mohiyeddini We have announced a workshop on healthcare burnout.
49% of doctors feel burned out in 83%, citing professional stress as the main contributor to burnout. Work-related “bureaucratic work” was identified as the main cause of burnout as too much time at work. Furthermore, women were more likely to report burnout feelings.
Another study with the Association of American Medical Colleges (AAMC) examined burnout, particularly among medical clinicians. It was found that 73% of respondents are burned out or at risk of burnout.
“People are called to medicine because they are hardworking and driven to help those who are responsible, their self-stars and those in need,” Morris said. “However, when practice conflicts with inner morality and compromises greatly on compliance with external demands that come with maintaining records, we can become exhausted, isolated, and permeate a sense of inefficiency… the burnout trio.”
They also spoke at length about moral injuries. Mohiyeddini described it as “a complex psychological state that is assumed to emerge after exposure to a disastrous event that challenges the moral values and ethical beliefs of an individual due to direct committees, omissions, observations, or betrayal by a trusted leader.”
“Transforming doctors into dr, drones, data entry experts and their own alternatives is a misuse of their talent and leads to moral injury,” Mohiedini said. “The 50% symptom rate of actual loss of pleasure, burnout, may be due to medical moral injury.”
So what happens when a healthcare worker is burning out or suffering from moral injuries?
Mohiyeddini explained that there are three elements in the psychology of burnout: Cognition; and behavior.
Emotional components can lead to energy depletion or fatigue. Cognition leads to increased mental distancing from one's job. And the behavioral components reduce occupational effectiveness (and are almost always leading to people with burnout being fired).
“The emotional element is usually the first thing people around you see,” Mohiyeddini said. “They'll see it before you realize it's there.”
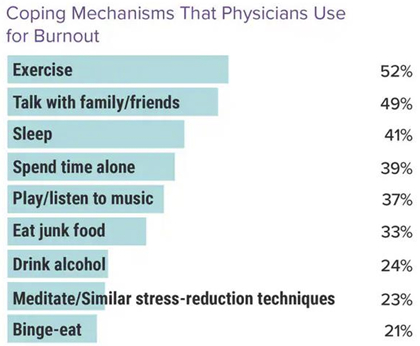
The pair identified several methods doctors use to deal with burnout. According to a Medscape report, exercise, discussions with family and friends, and sleep were the top mechanisms identified (see graphic for more details).
The doctor also dealt with burnout by changing the work environment. 32% reduced working hours, 25% changed work settings, or did different jobs, 22% changed workflows to facilitate workloads, and 21% spoke with managers about productivity pressure.
Additionally, 48% said the increase in compensation would be most helpful in burning out, followed by 47% suggesting adding support staff, and 46% recommending more flexible work schedules (respondents can choose up to three responses).
The two also suggested that individuals develop ways to improve resilience in several aspects.
“Elasticity means you don't fall very deep (to burnout) and recover faster,” Mohiyeddini said.
To work on improving cognitive resilience, Mohiyeddini suggested a simple exercise. Specifically, he urged people to carry small notebooks and pens and write down negative or challenging thoughts. (Don't pay attention to grammar etc.)
After about two hours (or when you feel good), go back to writing and read carefully. Then, erase any exaggerated, pessimistic, or motivating thoughts.
“Using this writing paradigm will help you identify and challenge negative thought patterns, ultimately leading to more positive and constructive thinking,” Mohiyeddini said.
By working on Resiliency, Mohiyeddini said health care providers are better at dealing with things that lead to burnout and moral injuries.
“Burnout is not an accident. You are the only person in charge of your mental health,” he said. “Build resilience.”
For more information, contact Andrew Mietderich, Senior Marketing Specialist at AT (Email Protection).
To request an interview, please visit the OUWB Communications & Marketing webpage.
This work is licensed under the Creative Commons Attribution-NonCommercial 4.0 International License.

