Breadcrumb Links
New Brunswick Health Issues
The union said the health network’s plan is not the right solution and that paying fair wages would solve the staff shortages.

Article Contents
A New Brunswick nursing home has become the centre of a furor over aged care as staff shortages have left it struggling to fill beds it added seven years ago.
Ad 2
Article Contents
Caught in the middle are administrators who don’t know where the new staff will come from, local health officials who want to redeploy hospital staff to nursing homes and labor unions who are unhappy with the planned changes.
Christine Corbett, administrator of the nonprofit Kiwanis Nursing Home in Sussex, said it would be great to have staff fully fill the 100 beds at the facility, which opened in 1979.
The home added 30 new beds in 2016 after an expansion that cost more than $11 million paid for by state taxpayers, but due to severe staffing shortages, Kiwanis has not been able to fill all of those beds, which typically leaves 20 to 25 beds unavailable.
“Sussex is a very small town and it’s very hard to find healthcare workers,” Corbett told Brunswick News. “It’s been a struggle ever since we expanded. There’s turnover so we have to be careful with our patient ratios in terms of staffing. We want to make sure our residents are safe and well cared for and our staff are safe and supported so we’re being very careful about that.”
In January, Corbett received word from the state Department of Social Development that Horizon Health Network, which runs the hospitals that see two-thirds of the state’s patients, was interested in redeploying some of its staff to the home, the first of its kind.
As you know, this situation is having a clear and direct impact on patient flow in hospitals and access to essential services such as emergency care and surgery.
Margaret Melancon
Horizon has its own problems: A third of its hospital beds are typically filled by elderly patients who are too frail to be discharged home. Most of them are on waiting lists for nursing homes. That creates acute-care bed shortages for other patients trying to get into emergency rooms and operating rooms.
Article Contents
Ad 3
Article Contents
“Our hospitals are facing significant and chronic capacity challenges, primarily due to an increase in acute care beds occupied by patients who no longer require inpatient care, a need that would be better met in long-term care settings,” Horizon CEO Margaret Melanson said in an email to Brunswick News. “As we know, this situation is having a clear and direct impact on patient flow through our hospitals and access to critical services such as emergency care and surgery.”
As a temporary measure to ensure elderly patients receive the right care in the right environment, Horizon is considering partnering with Kiwanis Nursing Homes to occupy and staff 25 long-vacant beds, he said.
“This is part of a broader effort to develop innovative, patient-centered models of care that improve access to acute care beds in our hospitals so patients can participate in activities, socialize and age in dignity in a safe, community-based environment,” she wrote.
But the plan has been confusing, particularly to the union that represents 4,600 care home workers.
That is not the right solution. The right solution is to pay fair wages and free up beds in nursing homes with staff.
Sharon Tear
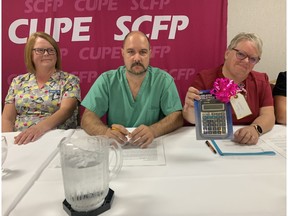
At a press conference last Wednesday, Sharon Teer, president of the New Brunswick Council of Nursing Home Unions, said the unions were not involved in developing the plan.
“We can’t recruit workers to help open beds because of the low wages,” she said at the Fredericton Inn. “This is unprecedented. And this is not the right solution. The right solution is to pay a fair wage so we can open beds with long-term care workers.”
Ad 4
Article Contents
The move comes amid a new collective bargaining impasse: The union is negotiating with the New Brunswick Nursing Homes Association, which takes its cues from the provincial government, which pays most of the workers’ pay.

The union claims Blaine Higgs’ Progressive Conservative government offered wage increases of about 12.5 per cent over four years, plus a $1.25 raise at the end of the contract, but the council, which is affiliated with the Canadian Union of Public Employees (CUPE), is seeking a flat-rate pay increase of $9 by the end of the new contract, which the union says is fairer to minimum-wage workers.
“We have a communal food pantry in the staff kitchen at our care home,” says Teare. “Do you know what that is? It’s a food bank. I heard yesterday that some staff actually use both the public food bank and their workplace food bank.”
During a photo op, one of the union’s top officials, council secretary-treasurer Bonnie Fournier, held up a new calculator that she said was a gift for Ernie Steeves, who served as finance minister in the Conservative government and is seeking re-election in the current election. Steeves recently announced a $500 million surplus for the fiscal year that ended March 31.
“When you look at the numbers, they don’t add up,” Fournier said. “Mr. Steves, if you use a new calculator, maybe you can come up with the right numbers.”
Ad 5
Article Contents
Teare thinks Horizon is problematic because unionized hospital workers typically earn higher wages than workers in nursing homes, which could mean two nursing home workers doing the same job would receive different wages.
The collective bargaining agreement for nursing home workers expired in October 2022. Resident caregivers, who do the majority of the work in nursing homes, earn between $21.74 and $23.41 an hour.
But hospital caregivers doing similar work, who earn between $22.60 and $25.11 an hour, according to their contracts, are also members of CUPE Local 1252, also known as the New Brunswick Council of Hospital Unions.
Kiwanis administrators, meanwhile, pointed to another problem: Help is already on the way. In March, representatives from Kiwanis Nursing Homes, along with five other homes from the province (Drew in Sackville, Loch Lomond Villa in Saint John, Orchard View in Gagetown, York Manor in Fredericton and Campbellton Nursing Home), embarked on a recruiting trip 13,000 kilometers across the globe to the Philippines.
Kiwanis alone is hiring 20 Filipino workers, 10 of whom she thinks could arrive as soon as November once the paperwork is complete. Once they’re all there, she said, all the beds in her home will be freed up.
The trip was organized by the provincial government, but it is unclear why the Department of Social Development sought to enter into an agreement with Horizon to transport hospital staff when the Filipinos’ arrival was imminent.
Ad 6
Article Contents
Brunswick News has asked the state government for an explanation, but the government has ignored the request.
Corbett said he was not aware of any discussions between Horizon, the department and the association.
“This is a state-level issue,” the administrator said, “and we’re not part of those discussions. But keep in mind this isn’t just about us. Our facility is unique in that we have free beds after our expansion, but there are facilities across the state that have free beds.”
Michael Keating, interim executive director of the New Brunswick Long-Term Care Home Association, said up to 200 beds are typically empty in long-term care homes across the province due to staff shortages.
We all know that hospitals are overflowing with patients waiting to enter nursing homes.
Michael Keating
But the hospital bed problem runs deeper: The province told Brunswick News last July that about 1,000 seniors were waiting to enter nursing homes, half of them in hospital beds.
“We all know that hospitals are overwhelmed with patients waiting to go into nursing homes,” Keating said, “so Horizon came up with the idea to fill Kiwanis beds with hospital patients.”
He said there was a lot of pushback from unions.
“CUPE correctly pointed out that this change would create income disparities among people working in the same setting. We have negotiated multiple times, but there were too many obstacles. That being said, the association will work with Kiwanis to see if we can move patients from hospitals to nursing homes.”
Article Contents
Share this article on social networks