Royal University of England (Rcseng). Future Surgery (RCSENG, 2018).
World Health Organization (WHO). Global Strategy for Digital Health 2020-2025 (World Health Organization, 2021).
House Open Committee. Digital Transformation of the NHS: 22-second report of the Session 2019-20 Report, and formal minutes (House of Commons Public Accounts Committee, 2020).
Scottish government. Digital Health and Care Strategy: Report from the External Expert Panel (Scottish Government, 2018).
Murray, E. Evaluating other digital health interventions: Key questions and approaches. morning. J. Previous. Pharmaceuticals. 51, 843–851 (2016).
NHS England Transformation Bureau. Digital Playbook, http://transform.england.nhs.uk/key-tools-info/digital-playbooks/ (2023).
McLean, KA, et al. Preparing for the implementation of new digital health interventions for postoperative monitoring: Systematic review and clinical innovation network analysis (CINA) according to the ideal framework. Lancet Digit. Health 5, E295 – E315 (2023).
Burke, Jr., Downey, C. &Almoudaris, Rescue Failures in Degraded Patients: A Systematic Review of Root Causes and Remediation Strategies. J. Patient SAF. 18, E140 – E155 (2022).
Efthymiou, CA&O'Regan, post-discharge complications: What exactly happens when a patient gets home? Let's interact. Heart vasc. Solek. Surgery. 12, 130–134 (2011).
World Health Organization (WHO). Telehealth: Opportunities and Development of Member States: Report on a Second Global Survey on EHealth (World Health Organization, 2010).
McLean, KA, et al. Implementation of digital remote postoperative surveillance in everyday practice: A qualitative study of barriers and facilitators. BMC Med. Let me know. Decided. Mac. 24, 307 (2024).
Esteva, A. Etal. Dermatologist-level classification of skin cancer with deep neural networks. Nature 542, 115–118 (2017).
Goodfellow, I., Bengio, Y. , & Courville, A. Deep Learning (Mit Press, 2016).
National Institutes of Health and Clinical Excellence (Nice). Quality Standard (QS113): Healthcare-related Infections (National Institute of Health and Clinical Excellence (NICE), 2016).
GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-, middle-, and low-income countries: a future international multicenter cohort study. Lancet infection. dis. 18, 516–525 (2018).
Astagneau, P., Rioux, C., Golliot, F., Brücker, G. &Inciso Network Study Group. Morbidity and mortality associated with surgical site infection: results of intravenous surveillance from 1997 to 1999. J. Hospital. infection. 48, 267–274 (2001).
Gheorghe, A. Etal. Health utility values related to surgical site infection: a systematic review. Value Health J. Int. Soc. Results of Pharmacoeconomics. 18, 1126–1137 (2015).
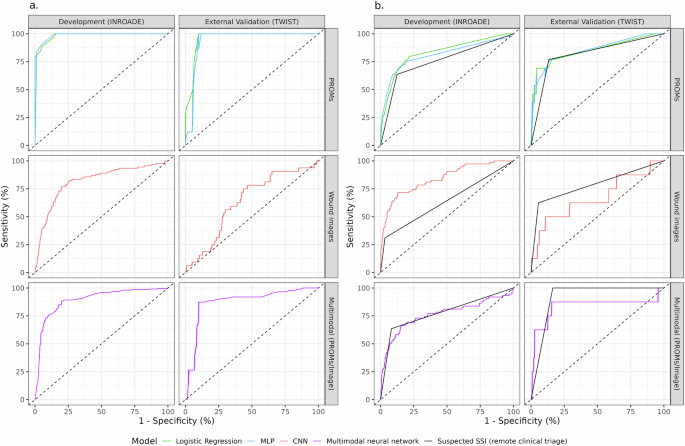
McLean, KA, et al. Remote diagnosis of surgical site infection using mobile digital interventions: a randomized controlled trial in emergency surgical patients. NPJ Digital MED. 4, 160 (2021).
McLean, KA, et al. Evaluation of remote digital postoperative wound monitoring in routine surgical practices. NPJ Digital MED. 6, 85 (2023).
Centers for Disease Control and Prevention (CDC) National Medical Safety Network (NHSN). Patient Safety Ingredients (PSC) Manual Chapter 9: Surgical Site Infection (SSI) Events (CDC, Atlanta, 2016).
McLean, K. Etal. Barriers and facilitators to the implementation of digital remote postoperative surveillance in everyday practice: a qualitative study. BMC Med. Let me know. Decided. Mac. 24, 307 (2024).
Rasan, R. Etal. Diagnostic accuracy of telemedicine for detection of surgical site infection: a systematic review and meta-analysis. NPJ Digital MED. 5, 108 (2022).
Reddy, Cl, Vervoort, D., Meara, J.G. & Atun, R. Surgery and Universal Health Coverage: Key package design for expansion and scale-up of surgical care. J. Glove. Health 10, 020341 (2020).
Covidsurg Collaborative. Cancellation of elective surgeries due to the Covid-19 pandemic: Global predictive modeling to inform surgical recovery plans. br. J. Surgery. 107, 1440–1449 (2020).
Google Scholar
Whisokki, O. Etal. Evaluating the communication gap between AI models and healthcare professionals: explainability, usefulness, and trust in AI-driven clinical decision-making. artif. Intel. 316, 103839 (2023).
Quinn, T. P., Senadeera, M., Jacobs, S., Coghlan, S. & Le, V. Trust and Medical AI: The challenges we face and the expertise we need to overcome them. J. Am. Med Inf. Association. 28, 890–894 (2021).
Richardson, JP, et al. Patient anxiety regarding the use of artificial intelligence in healthcare. NPJ Digital MED. 4, 140 (2021).
Shenoy, V. N., Foster, E., Aalami, L., Majeed, B. & Aalami, O. Deepwound: Automated postoperative wound assessment and surgical site monitoring through a convolutional neural network. IEEE International Conference on Bioinformatics and Biomedical Sciences (BIBM). 1017–1021 (IEEE, 2018).
Kaundinya, T. & Kundu, Diversity of Skin Images in RV Medical Texts: Recommendations for Student Advocacy in Medical Education. J. Med Educ. Curriculum. Developer. 8, 23821205211025855 (2021).
Guo, LN, Lee, M. S., Kassamali, B., Mita, C. & Nambudiri, Ve Bias in, Bias Out: Underreporting and Underestimating a Diverse Skin Type in Machine Learning Research for Skin Cancer Detection – A Scoping Review. J. Am. Academy. Dermatore. 87, 157–159 (2022).
Choi, D. Etal. Development of machine learning models that estimate weekly US suicide killing using multiple heterogeneous data sources. Jamanet. Open 3, E2030932 (2020).
Rasmy, L. Etal. Recurrent Neural Network Model (COVRNN) to Predict COVID-19 Patient Outcomes upon Hospital Admission: Model Development and Validation Using Electronic Health Record Data. Lancet Digital Health 4, E415 – E425 (2022).
Choi, E., Schuetz, A., Stewart, W. F. & Sun, J. J. Am. Med Inf. Association. 24, 361–370 (2017).
van Royen, FS, Moons, KGM, Geersing, G.-J. & Van Smeden, M. Develop, validate, update and determine the impact of prognostic models on respiratory disease. EUR. response. J. 60, 2200250 (2022).
Ian, A.S., Stacy, MC & Enrico, C. Exploring stakeholder attitudes towards AI in clinical practice. BMJ Healthcare Information. 28, E100450 (2021).
Hogg, Hdj et al. Stakeholder perspectives in implementing clinical artificial intelligence: a systematic review of qualitative evidence. J. Med. Internet resolution. 25, E39742 (2023).
Daneshjou, R. Etal. Dermatology Difference AI is the performance of a diverse and curated set of clinical images. SCI. Adv. 8, EABQ6147 (2022).
Transparent report (tripod) of multivariable predictive models for individual prognosis or diagnosis of Collins, GS, Reitsma, JB, Altman, DG & Moons, KGM Transparent report (tripod) of multivariable predictive models for individual prognosis or diagnosis: a tripod statement. BMC Med. 13, 1 (2015).
An integrated workflow that develops, evaluates and outputs prediction models for McLean, K., Knight, Sr, Harrison, EM Predictr:R, http://github.com/kamclean/predictr (2022).
Fischer, J.E., Bachmann, L.M. & Jaeschke, R. Reader's Guide to Interpretation of Diagnostic Test Properties: Clinical Cases of Sepsis. Intensive care medication. 29, 1043–1051 (2003).
Menzies, T., Kocagüneli, E., Minku, L., Peters, F. & Turhan, B. Software Engineering Data and Model Sharing (Eds Tim Menzies et al.) 321–353 (Morgan Kaufmann, 2015).
Shin, HC, etc. Deep convolutional neural networks for computer-aided detection: CNN architecture, dataset characteristics, and transfer learning. IEEE Transformer. MED Imaging 35, 1285–1298 (2016).
Sánchez-Cauce, R., Pérez-Martín, J. &Luque, M. A multi-input convolutional neural network for breast cancer detection using thermal imaging and clinical data. computer. Method Prog. Biomed. 204, 106045 (2021).
Nguyen, T. & Pernkopf, F. Crackle detection of lung sounds using transfer learning and multi-input convolutional neural networks. The 43rd International Conference on IEEE Engineering at the 43rd Society for Medical and Biomedical Sciences (EMBC). 80–83 (IEEE, 2021).
National Health Services England. How can I calculate the FTE/WTE required for a role? (National Health Services England, 2024).