Baseline characteristics
In total, 6123 patients age 16 and older were extracted from three different common practices. 143 patients were excluded due to missing data, leaving 5980 patients in the study population. The survey response rate was 39% (n = 2361). The baseline characteristics of participants and nonresponders are shown in Table 1. The median age of participants was higher than that of nonresponders (median 57 years, (16-93) vs. 40 years (16-93)). Furthermore, the proportion of women was higher in the participant group (58%) compared to the non-responsive group (44%). Patients with hypertension, heart failure, and malignant tumors showed a higher response rate. In contrast, people with asthma or COPD had a lower response rate. A lower response rate was observed in individuals identified as having symptoms of COVID-19 by the AI model.
COVID-19 Symptoms
According to the AI model, out of 5,980 patients, 4,207 have been in contact with GP at least once for a variety of reasons. Information on Covid-19 was found in 3,400 unique medical records, of which 1,508 patients participated in the survey. In the 1660 medical records, the AI model predicted the existence of Covid-19. 41.9% of this group participated in the survey.
Of all participants, 23% (n = 535) reported experiencing Covid-19-related symptoms (Table 2). Of these, 139 participants (26%) actually took a positive PCR test by testing with community health services. The most frequently reported symptoms were cough (56%), fever (56%), dyspnea (51%), cold (51%), and muscle pain (50%). Of these, 180 participants (33.6%) reported seeking Covid-19 help, and 176 contacted the GP. Four patients went directly to the hospital without involvement of GP. Of the 535 participants who had complaints during the first wave, 236 (44%) reported persistent complaints. Within this group, 80 participants (15%) reported experiencing symptoms for more than 24 months.
There was no significant difference in the proportion of relatives and acquaintances who experienced severe Covid-19 symptoms or died before their illness among participants. As mentioned in the free text section of the survey, it included “Because of the wave of participants,” “We were waiting at home to reduce the severity of the complaints to a level that is tolerated,” and “the government advice at the time was to only seek help if you were severely short of breath.”
Theme Analysis Semi-structured Interview
Data saturation was reached after interviewing 12 participants. Twenty patients were invited and 12 were interviewed to reach saturation. The median age of the 12 interviewees was 57 years (range 38-80 years), and generally rated their health as reasonably good (Table 3). Five interviewees (42%) had relatives who had experienced or died of severe Covid-19 symptoms. The average interview period was 20 minutes, with major themes such as mental, physical, social, and care use (Figure 2).
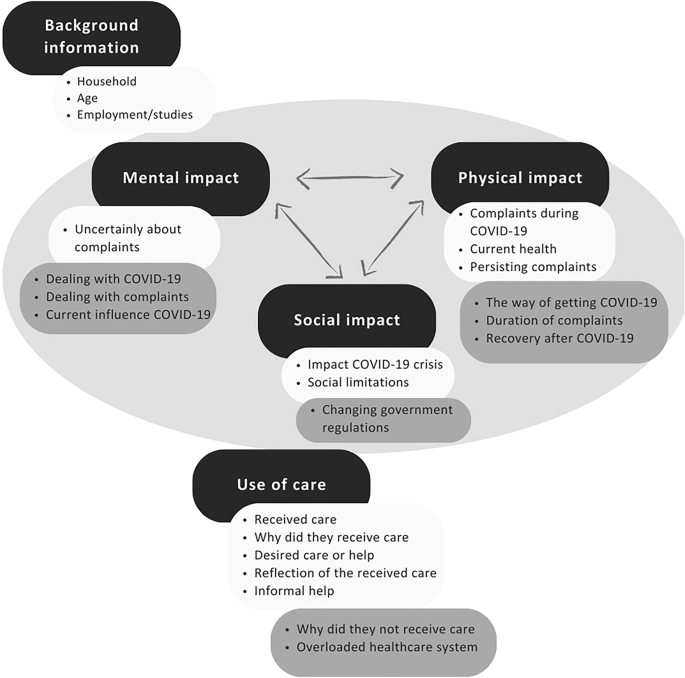
Cross-sectional theme networks of interrelated themes before the interview (light gray) and additional themes arising from the qualitative analysis of the interview (n = 12).
Physical influences
The main reason they were not seeking help was the assumption that participants were not seriously ill. One participant (#1) said: I don't go to GP very often. In fact, to put that in a different way, I rarely go. If I went, there's a good reason for that, and feeling like I'm sick for 3 weeks and flu doesn't necessarily mean I'll talk to my doctor. One participant showed that he was experiencing a continuous complaint, but at that point he didn't want to put too much strain on his GP because of the high workload of his GP. Participant #5 reflects on the challenging situation of GPS. But the knowledge that GPs were in such a crisis and were extremely busy, has heard one after another death bell after another after you actually arrived. He showed some things they would have asked for help if the symptoms had lasted a little longer.
Mental impact
The mental impact was primarily attributed to the broader COVID-19 crisis in general. Several participants described Hasselt's deaths as extremely shocking and intense. Some older participants noted that the infection and crisis had less overall impact as they have already retired and engaged in less activity. Participant #3 states: Influenza also passes, so I think this will pass too. And I have a wife who can intervene whenever necessary, so why do I need special care?
Social impact
Participants frequently cited changes in social limitations and social interactions as important factors. Participants (#6) also commented on difficult social limitations, but added. But on the other hand, the vast number of people around you have died, and everyone has friends and acquaintances. Furthermore, many participants expressed their dissatisfaction with the lack of clarity from the central government and frequent changes in Covid-19 regulations, noting that clearer communication may have alleviated these issues. One participant (#4) mentions the lack of appropriate resources to provide adequate care. But the fact that while everything in Hasselt is infected, it takes a very long time to realize that he has COVID. If they had just tested everyone back then it would have been much more accurate. And while you could have done targeted behavior, you were a little confused now.
Care Use
Participants expressed a variety of preferences for support and care. I wanted more support from the GP, but I was facing barriers like limited complaints and GP workloads. They also highlighted bottlenecks in the health care system that have been exacerbated by COVID-19, including limitations in PCR testing capabilities and inadequate aftercare for long-term COVID-19 effects. The suggestions for improvement included a 24-hour helpline and better guidance on complaints and medication use.
Overall, various factors contributed to participants' self-direction and self-control. Their acceptance of illness and the inability to visit GPs was a common theme. Furthermore, the majority experienced voluntary improvement through rest. One participant (#5) explained the situation as follows: I am actively surprised by my ability to deal with it, and also trusting the signals my body was giving me, and when I think about it, I am sick, I am very sick, but not too sick. I'm in control so at this time there's no need for a caregiver.
Informal support from partners or children, including task support and emotional support, helped self-management. Participants highly valued healthcare workers despite the challenges involved in arranging immediate assistance. Although they wanted several different outcomes, many understood the constraints of the crisis and did not condemn GPS. Looking ahead, Participant 5 stated: Look, if you have it now, I would rather talk directly to the GP. That little consultation, but it simply wasn't there at the time either.

