Osamor, P., Grady, C. Factors associated with women’s health care decision-making autonomy: empirical evidence from Nigeria. J. Biosoc Sci. 50 (1), 70–85 (2018).
Google Scholar
Sano, Y. et al. Married women’s autonomy and post-delivery modern contraceptive use in the Democratic Republic of congo. BMC Womens Health. 18 (1), 49 (2018).
Google Scholar
Alemayehu, M. & Meskele, M. Health care decision making autonomy of women from rural districts of Southern Ethiopia: a community based cross-sectional study. Int. J. Womens Health. 9, 213–221 (2017).
Google Scholar
Asabu, M. D. & Altaseb, D. K. The trends of women’s autonomy in health care decision making and associated factors in Ethiopia: evidence from 2005, 2011 and 2016 DHS data. BMC Womens Health. 21 (1), 371 (2021).
Google Scholar
Ahmed, S. et al. Autonomous decision-making for antenatal screening in Pakistan: views held by women, men and health professionals in a low–middle income country. Eur. J. Hum. Genet. 27 (6), 848–856 (2019).
Google Scholar
Yount, K. M., Dijkerman, S., Zureick-Brown, S. & VanderEnde, K. E. Women’s empowerment and generalized anxiety in Minya, Egypt. Soc. Sci. Med. 106, 185–193 (2014).
Google Scholar
Couva, M., Talias, M. A., Christou, M. & Soteriades, E. S. Women’s empowerment and health: A narrative review. Int. J. Environ. Res. Public. Health 21 (12), 1614 (2024).
Google Scholar
Anderson, R. M. & Funnell, M. M. Patient empowerment: Myths and misconceptions. Patient Educ. Couns. 79 (3), 277–282 (2010).
Google Scholar
United Nations Population Fund. Ensure universal access to sexual and reproductive health and reproductive rights (Internet). 2020 (cited 2024 Dec 15). https://www.unfpa.org/sites/default/files/pub-pdf/UNFPA-SDG561562Combined-v4.15.pdf.
Idris, I. B. et al. Women’s autonomy in healthcare decision making: a systematic review. BMC Womens Health 23 (1), 643 (2023).
Google Scholar
Acharya, D. R., Bell, J. S., Simkhada, P., van Teijlingen, E. R. & Regmi, P. R. Women’s autonomy in household decision-making: a demographic study in Nepal. Reprod. Health. 7 (1), 15 (2010).
Google Scholar
Kamiya, Y. Women’s autonomy and reproductive health care utilisation: empirical evidence from Tajikistan. Health Policy (New York) 102 (2–3), 304–313 (2011).
Google Scholar
Self, S. & Grabowski, R. Female autonomy and health care in developing countries. Rev. Dev. Econ. 16 (1), 185–198 (2012).
Google Scholar
Woldemicael, G. Do women with higher autonomy seek more maternal health care?? Evidence from Eritrea and Ethiopia. Health Care Women Int. 31 (7), 599–620 (2010).
Google Scholar
Woldemicael, G. & Tenkorang, E. Y. Women’s autonomy and maternal Health-Seeking behavior in Ethiopia. Matern Child. Health J. 14 (6), 988–998 (2010).
Google Scholar
Tiruneh, F. N., Chuang, K. Y. & Chuang, Y. C. Women’s autonomy and maternal healthcare service utilization in Ethiopia. BMC Health Serv. Res. 17 (1), 718 (2017).
Google Scholar
Awoleye, A. F., Victor, C. & Alawode, O. A. Women autonomy and maternal healthcare services utilization among young ever-married women in Nigeria. Int. J. Nurs. Midwifery 10 (6), 62–73 (2018).
Ameyaw, E. K., Tanle, A., Kissah-Korsah, K. & Amo-Adjei, J. Women’s health Decision-Making autonomy and skilled birth attendance in Ghana. Int. J. Reprod. Med. 2016, 6569514 (2016).
Google Scholar
Hindin, M. J., WOMEN’S AUTONOMY, S. T. A. T. U. S. & NUTRITION IN ZIMBABWE, Z. A. M. B. I. A. AND AND MALAWI. Women’s Autonomy, Status, and Nutrition. ;93–116. (2005).
Haque, R., Alam, K., Rahman, S. M., Keramat, S. A. & Al-Hanawi, M. K. Women’s empowerment and fertility decision-making in 53 low and middle resource countries: a pooled analysis of demographic and health surveys. BMJ Open. 11 (6), e045952 (2021).
Google Scholar
Tanyag, M. Sexual and reproductive health is a security issue for Southeast Asia. Australian J. Int. Affairs. 72 (6), 495–499 (2018).
Google Scholar
Sohn, M. & Jung, M. Effects of empowerment and media use by women of childbearing age on maternal health care utilization in developing countries of Southeast Asia. Int. J. Health Serv. 50 (1), 32–43 (2020).
Google Scholar
Sebayang, S. K., Efendi, F. & Astutik, E. Women’s empowerment and the use of antenatal care services: analysis of demographic health surveys in five Southeast Asian countries. Women Health. 59 (10), 1155–1171 (2019).
Google Scholar
Nafiah, I., Samosir, O. B., Sastiono, P., ACHIEVING THE SDGs & TARGETS: WOMEN’S AUTONOMY AND THE CONTINUUM OF MATERNAL AND CHILD HEALTH SERVICES UTILIZATION IN INDONESIA USING IDHS 2017. J. Environ. Sci. Sustainable Dev. 5(2). (2022).
Wirawan, G. B. S. et al. Women’s empowerment facilitates complete immunization in Indonesian children: A Cross-sectional study. J. Prev. Med. Public. Health. 55 (2), 193–204 (2022).
Google Scholar
Rizkianti, A., Afifah, T., Saptarini, I. & Rakhmadi, M. F. Women’s decision-making autonomy in the household and the use of maternal health services: an Indonesian case study. Midwifery 90, 102816 (2020).
Google Scholar
Osamor P, Grady C. Women’s autonomy in health care decision-making in developing countries: a synthesis of the literature. Int J Womens Health. 191 (2016).
Griselda, M., Alfian, S. D., Wicaksono, I. A., Wawruch, M. & Abdulah, R. Findings from the Indonesian family life survey on patterns and factors associated with Multimorbidity. Sci. Rep. 13 (1), 18607 (2023).
Google Scholar
Hussain, M. A., Huxley, R. R. & Al Mamun, A. Multimorbidity prevalence and pattern in Indonesian adults: an exploratory study using National survey data. BMJ Open. 5 (12), e009810 (2015).
Google Scholar
National Population and Family Planning Board (BKKBN). Statistics Indonesia (BPS), Ministry of Health (Kemenkes), ICF. Indonesia Demographic and Health Survey 2017. Jakarta & Rockville: BKKBN, BPS, Kemenkes, and ICF. (2018).
The DHS Program. Protecting the Privacy of DHS Survey Respondents (Internet). 2014 (cited 2023 Jun 20). https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm.
Alem, A. Z. et al. Timely initiation of antenatal care and its associated factors among pregnant women in sub-Saharan Africa: A multicountry analysis of demographic and health surveys. PLoS One 17 (1), e0262411 (2022).
Google Scholar
Ameyaw, E. K., Seidu, A. A. & Ahinkorah, B. O. Women’s healthcare decision-making and unmet need for contraception in Mali. Reprod. Health 19 (1), 183 (2022).
Google Scholar
Negash, W. D., Kefale, G. T., Belachew, T. B. & Asmamaw, D. B. Married women decision making autonomy on health care utilization in high fertility sub-Saharan African countries: A multilevel analysis of recent demographic and health survey. PLoS One 18 (7), e0288603 (2023).
Google Scholar
Tsehay, C. T. Factors associated with modern contraceptive demands satisfied among currently married/in-union women of reproductive age in Ethiopia: a multilevel analysis of the 2016 demographic and health survey. BMJ Open. 12 (2), e049341 (2022).
Google Scholar
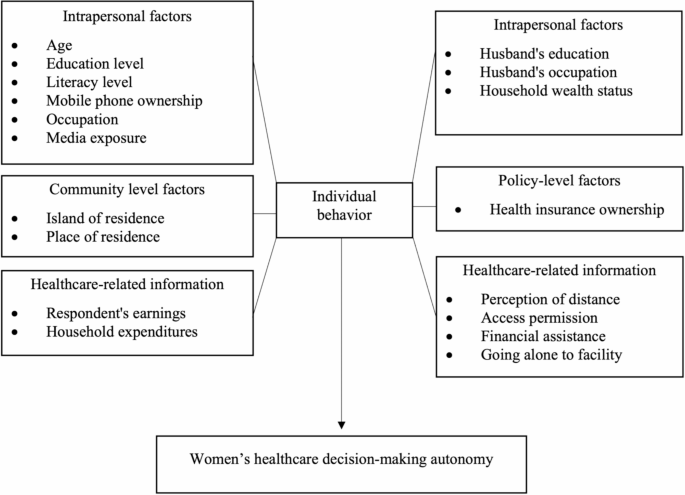
Sallis, J. F. O. N. F. E. Chapter 20: Ecological models of heath behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4th ed. San Francisco (2008).
McLeroy, K. R. B. D. S. A. G. K. An ecological perspective on health promotion programs. Health Educ. Q. (15 (4), 351–377 (1988).
Google Scholar
Hardhantyo, M. & Chuang, Y. C. Urban-rural differences in factors associated with incomplete basic immunization among children in Indonesia: A nationwide multilevel study. Pediatr. Neonatol. 62 (1), 80–89 (2021).
Google Scholar
Kim, J. H. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 72(6):558. https://pmc.ncbi.nlm.nih.gov/articles/PMC6900425/ (2019).
Chowdhury, M. Z. I. & Turin, T. C. Variable selection strategies and its importance in clinical prediction modelling. Fam Med. Community Health 8 (1), e000262 (2020).
Google Scholar
Bursac, Z., Gauss, C. H., Williams, D. K. & Hosmer, D. W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 3 (1), 17 (2008).
Google Scholar
Mullany, B. C. Spousal agreement on maternal health practices in Kathmandu, Nepal. J. Biosoc Sci. 42 (5), 689–693 (2010).
Google Scholar
Mare, K. U., Aychiluhm, S. B., Tadesse, A. W. & Abdu, M. Married women’s decision-making autonomy on contraceptive use and its associated factors in Ethiopia: A multilevel analysis of 2016 demographic and health survey. SAGE Open. Med. 10, 205031212110687 (2022).
Nadeem, M., Malik, M. I., Anwar, M. & Khurram, S. Women decision making autonomy as a facilitating factor for contraceptive use for family planning in Pakistan. Soc. Indic. Res. 156 (1), 71–89 (2021).
Google Scholar
Rajkhowa, P. & Qaim, M. Mobile phones, women’s physical mobility, and contraceptive use in India. Soc. Sci. Med. 305, 115074 (2022).
Google Scholar
Rotondi, V., Kashyap, R., Pesando, L. M., Spinelli, S. & Billari, F. C. Leveraging mobile phones to attain sustainable development. Proc. Natl. Acad. Sci. 117 (24), 13413–13420 (2020).
Google Scholar
Ahmed, S., Creanga, A. A., Gillespie, D. G. & Tsui, A. O. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One 5 (6), e11190 (2010).
Google Scholar
Fotso, J. C., Ezeh, A. C. & Essendi, H. Maternal health in resource-poor urban settings: how does women’s autonomy influence the utilization of obstetric care services? Reprod. Health 6 (1), 9 (2009).
Google Scholar
Story, W. T. & Burgard, S. A. Couples’ reports of household decision-making and the utilization of maternal health services in Bangladesh. Soc. Sci. Med. 75 (12), 2403–2411 (2012).
Google Scholar
Beegle, K., Frankenberg, E. & Thomas, D. Bargaining power within couples and use of prenatal and delivery care in Indonesia. Stud. Fam Plann. 32 (2), 130–146 (2001).
Google Scholar
Zegeye, B. et al. Association between women’s household decision-making autonomy and health insurance enrollment in sub-saharan Africa. BMC Public. Health 23 (1), 610 (2023).
Google Scholar
Furuta, M. & Salway, S. Women’s position within the household as a determinant of maternal health care use in Nepal. Int. Fam Plan. Perspect. 32 (01), 017–27 (2006).
Google Scholar
von Elm, E. et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335 (7624), 806–808 (2007).
Google Scholar
Kassahun, A. & Zewdie, A. Decision-making autonomy in maternal health service use and associated factors among women in Mettu district, Southwest Ethiopia: a community-based cross-sectional study. BMJ Open. 12 (5), e059307 (2022).
Google Scholar
Haque, S. E., Rahman, M., Mostofa, M. G. & Zahan, M. S. Reproductive health care utilization among young mothers in Bangladesh: does autonomy matter? Womens Health Issues 22 (2), e171–e180 (2012).
Google Scholar
Conzo, P., Fuochi, G. & Mencarini, L. Fertility and life satisfaction in rural Ethiopia. Demography 54 (4), 1331–1351 (2017).
Google Scholar
Senarath, U. & Gunawardena, N. S. Women’s autonomy in decision making for health care in South Asia. Asia Pac. J. Public. Health 21 (2), 137–143 (2009).
Google Scholar
Seidu, A. A. et al. Women’s autonomy in household decision-making and safer sex negotiation in sub-Saharan Africa: an analysis of data from 27 demographic and health surveys. SSM Popul. Health 14, 100773 (2021).
Google Scholar
BPS-Statistics Indonesia. Number of General Hospitals, Special Hospitals, and Public Health Centers (Unit), 2014–2015 (Internet). 2015 (cited 2024 Dec 24). https://www.bps.go.id/en/statistics-table/2/MjMyIzI=/number-of-general-hospitals–special-hospitals–and-public-health-centers–unit-.html.
Widiastuti, W. Domestic tourism in Indonesia: another story of inequality between Java and Non-Java. J. Indonesian Tourism Dev. Stud. 8 (1), 45–49 (2020).
Rofita, D., Makmun, I., Amilia, R., Lestari, C. I. & Sofiatun, S. Factors affecting child marriage in West Nusa Tenggara. Jurnal Promosi Kesehatan Indonesia 18 (1), 16–24 (2022).
Gebeyehu, N. A. et al. Women decision-making autonomy on maternal health service and associated factors in low- and middle-income countries: Systematic review and meta-analysis. Women’s Health (Internet). 2022 Sep 3 (cited 2025 Feb 14);18. https://journals.sagepub.com/doi/https://doi.org/10.1177/17455057221122618.
Green, S. H., Wang, C., Ballakrishnen, S. S., Brueckner, H. & Bearman, P. Patterned remittances enhance women’s health-related autonomy. SSM Popul. Health 9, 100370 (2019).
Google Scholar
Ghose, B. et al. Women’s decision-making autonomy and utilisation of maternal healthcare services: results from the Bangladesh demographic and health survey. BMJ Open. 7 (9), e017142 (2017).
Google Scholar
Belvedere, L. M., Davis, S. F., Gray, B. L. & Crookston, B. T. Improvements to female autonomy and household Decision-Making power from an intervention targeting improved food security: A Gender-Based analysis of the Rajasthan nutrition project. Health N Hav. 13 (02), 188–203 (2021).
Olwanda, E. et al. Women’s autonomy and maternal health decision making in Kenya: implications for service delivery reform – a qualitative study. BMC Womens Health 24 (1), 181 (2024).
Google Scholar
Sharma, S., Mehra, D., Akhtar, F. & Mehra, S. Evaluation of a community-based intervention for health and economic empowerment of marginalized women in India. BMC Public. Health 20 (1), 1766 (2020).
Google Scholar
Desai, S. et al. Community interventions with women’s groups to improve women’s and children’s health in India: a mixed-methods systematic review of effects, enablers and barriers. BMJ Glob Health 5 (12), e003304 (2020).
Google Scholar