In response to hospital capacity challenges brought on by the COVID-19 pandemic, the Centers for Medicare and Medicaid Services (CMS) is collaborating with outside experts to improve home acute hospital care (AHHCAH). Founded the initiative. The initiative expires Dec. 31 unless Congress extends it. After three years of implementation, early insights into quality, cost, and care have begun to shape the future of this program and initiatives like it.
CMS originally launched the Hospitals Without Walls initiative in March 2020, using authority under the Social Security Act that allows the Secretary of Health and Human Services to waive or modify certain facility standards during public health emergencies. Ta.
Building on this effort, CMS introduced the AHCAH program in November 2020. This program allows acute care hospitals that receive payments under the Inpatient Prospective Payment System to expand their provision of inpatient home care.
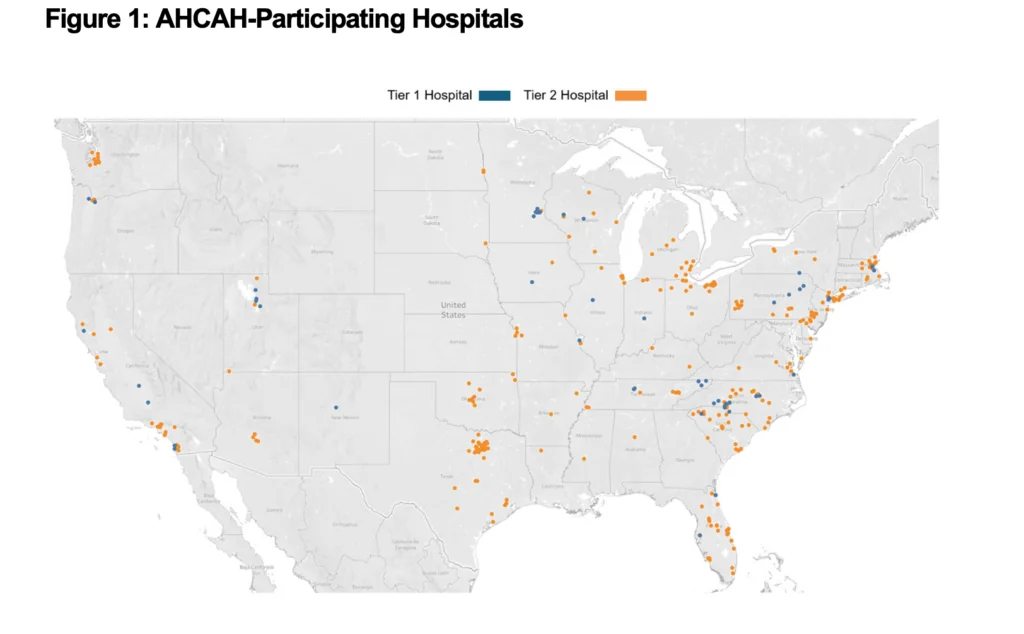
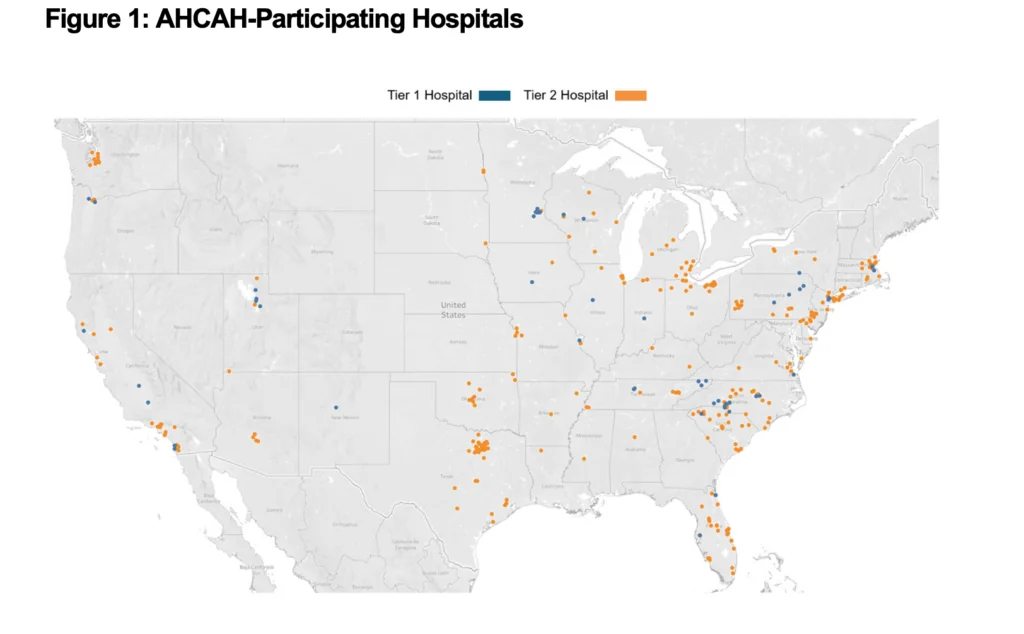
To participate in this effort, hospitals must submit a waiver request through a dedicated CMS portal. After review, CMS will meet with each requesting hospital to evaluate the hospital's ability to provide high-quality, safe care in the home setting in accordance with the Medicare Hospital Participation Conditions. Once approved, hospitals will be able to provide inpatient treatment to eligible patients in their own homes. As of October 2024, 366 hospitals have participated in the initiative, serving more than 31,000 patients in a home setting, according to CMS.
In December 2022, Congress passed the Consolidated Appropriations Act of 2023 (CAA), extending the AHCAH initiative until December 31, 2024. The CAA also required CMS to conduct a study to evaluate several aspects of the initiative. As a result of this study, the AHCAH Initiative Research Report was published on September 30, 2024.
This study used the best available quantitative and qualitative data to compare patients at AHCAH with those admitted to traditional brick-and-mortar hospitals. The comparison included 332 participating hospitals in 38 states and covered the period from November 2020 to July 2024. Data analysis focused on several key areas including patient participation criteria and demographics, clinical conditions treated, quality of care, cost and service utilization, and patient experience. .
Patient demographics
Each hospital established patient acceptance criteria based on its experience and resources to provide inpatient-level care in a home setting. This standard also incorporates nationally recognized standards. Specific selection criteria considered clinical and psychosocial factors, home environment, and patient willingness to participate.


The analysis revealed significant differences between patients treated at home (AHCAH patients) and those admitted to traditional inpatient facilities from the same hospital. AHCAH patients were more likely to be white, live in an urban area, and less likely to be a Medicaid recipient.
Comparison of quality of care
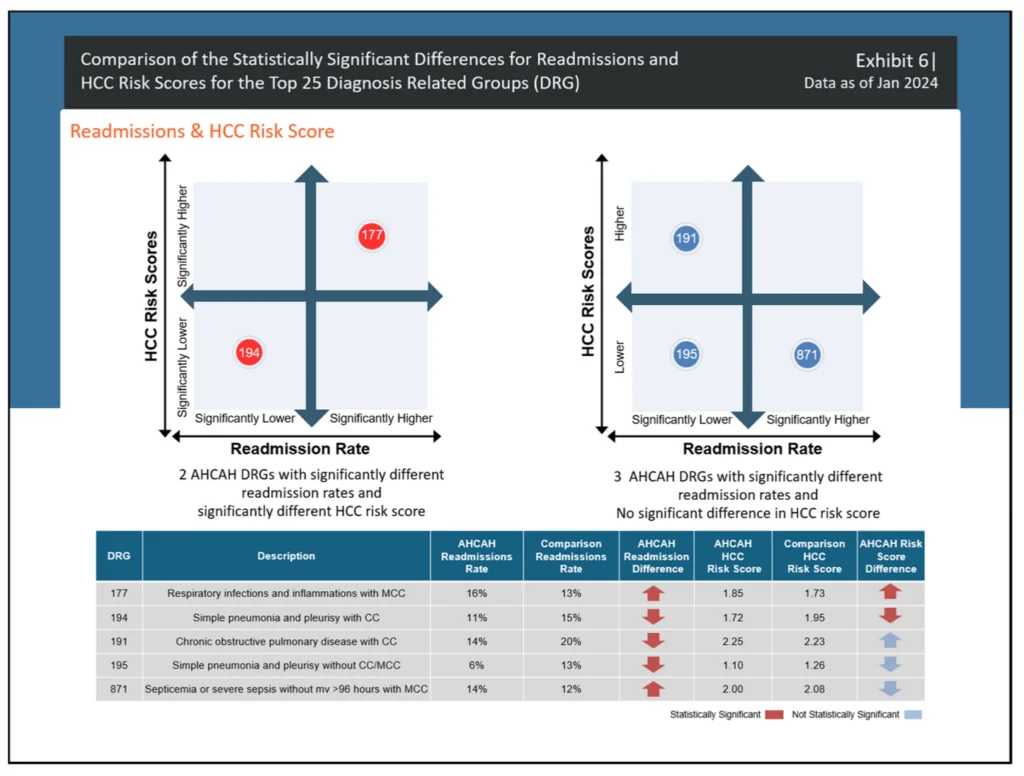
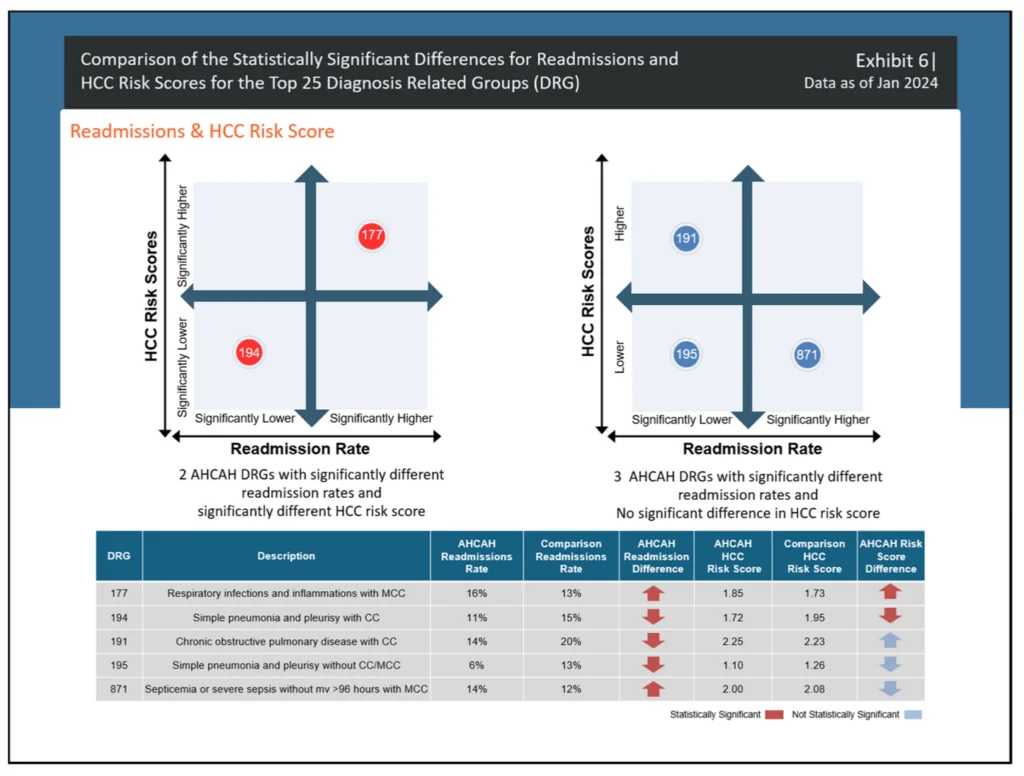
This study used the Medicare Severity Diagnosis-Related Group (MS-DRG) and Major Diagnostic Category (MDC) classification systems to identify the most common diseases treated through the AHCAH initiative. The results showed that the main symptoms were respiratory diseases, cardiovascular diseases, kidney diseases, and infections.
To compare quality of care, three quality indicators were analyzed: 30-day mortality rate, 30-day readmission rate, and nosocomial infection rate. AHCAH beneficiaries generally had lower 30-day mortality rates than traditional hospitalized patients, according to CMS.
However, the AHCAH group had significantly higher readmission rates for two specific MS-DRGs: respiratory infections and inflammation requiring mucociliary removal, and sepsis without mechanical ventilation or severe sepsis. It was expensive. Conversely, the other three MS-DRGs, i.e., simple pneumonia and pleurisy with complications or comorbidities, simple pneumonia and pleurisy without complications, comorbidities, or need for mucociliary removal; Chronic obstructive pulmonary disease with symptoms or comorbidities had significantly lower readmission rates.
From a cost perspective, CMS evaluated the impact on Medicare program spending rather than individual hospital costs. Analysis of inpatient care episodes from admission to discharge revealed that AHCAH episodes resulted in an average of less than 1 day of extra hospital stay. Additionally, AHCAH beneficiaries had significantly lower Medicare spending in the 30 days after hospital discharge.
patient experience
Qualitative data on patient experiences under the AHCAH initiative were collected through listening sessions, site visits, and informal interviews with caregivers. The findings indicate that both patients and caregivers who shared feedback had positive experiences with the care provided through this initiative. This is broadly consistent with the positive patient experience results associated with hospital-at-home programs.
Clinicians who participated in this initiative also reported primarily positive experiences.
Early lessons from the AHCAH initiative suggest that health care providers can provide safe, high-quality inpatient care in a home setting for appropriately selected patients. This approach aligns with and supports the CMS Center for Clinical Standards and Quality's core mission of improving lives, health outcomes, and the experience of care.
The initiative expires on Dec. 31, so important questions remain. CMS is reportedly exploring opportunities to address these questions if the program is extended.

