Study design
This study is a prospective observational pilot study evaluating the feasibility, cost-effectiveness, and impact of a mobile telemedicine system in underserved rural areas of Hungary. Rather than strictly following a predefined telemedicine or healthcare delivery framework, we adapted our approach to the specific challenges and needs of the target population to maximize effectiveness. Our methodology was shaped by practical considerations and real-world constraints, ensuring that the intervention was both feasible and responsive to the local healthcare landscape. The study was conducted over a six-month period (April–October 2023), assessing healthcare utilization, new diagnoses, and patient&doctor satisfaction.
The districts included in this study were selected from the 300 officially designated FeTe areas, which have been identified by the Hungarian Government and international organizations as the most socioeconomically disadvantaged regions. This externally validated classification ensured that the intervention targeted communities with the greatest documented need, while also mitigating potential bias in site selection. By focusing on these areas, we aimed to provide healthcare services where they were most urgently required, aligning with national and EU-supported socioeconomic development strategies.
Description of intervention
The mobile healthcare units were centrally operated from a single base in central Hungary, from where all vehicles departed each morning and returned the same day, covering an average of 500 km per trip. The target settlements were often difficult to access, with road conditions varying significantly between regions, impacting travel efficiency and scheduling.
A further challenge was ensuring stable internet connectivity for telemedicine consultations. The mobile network bandwidth varied across locations, influenced by both geographic factors and weather conditions, occasionally affecting data transmission quality.
Additionally, the diagnostic tools used in the intervention were originally designed for stationary use, making their daily transportation a logistical concern. Special precautions were required to prevent vibration, moisture exposure, and temperature fluctuations, ensuring that sensitive medical devices remained functional and accurate throughout the intervention.
Despite these challenges, operational adjustments, scheduling optimizations, and equipment protection protocols were implemented to maintain service quality and minimize disruptions.
Description of the examined area
The introduction of our telemedicine system took place between April and October in 2023. The examined population came from 30 different locations, rural FeTe villages which constitute 5 districts, situated around 5 centers of telemedicine services. The 5 centers are the villages of Zalakomar, Hirics, Litke, Szalonna and Nyirkata (Fig. 1). Hereafter, the involved 5 districts and project together will be referred as “Programme”. The Programme served as the healthcare component of the socioeconomic development program in the FeTe settlements. To investigate the effectiveness of the nationwide telemedicine system, a preliminary analysis of population has been carried out.
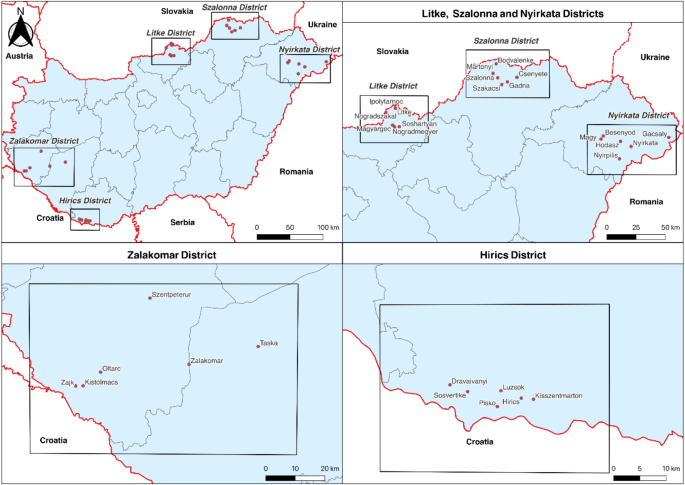
Districts involved in the programme. This figure shows the five rural Hungarian districts involved in the telemedicine programme: Zalakomar, Hirics, Litke, Szalonna, and Nyirkata. The map highlights these areas where mobile healthcare service centers (MHSCs) were deployed to provide medical services to underserved populations.
Total population size of the five districts was 21,477 based on the 2022 Hungarian census. The control population was selected from other FeTe settlements based on their similar geographical location, socio–economic and demographic characteristics, but without Maltese Health Point (MHP) availability. MHP is a place that offers regular health service – telemedicine or traditional practice – and is operated and maintained by the Hungarian Charity Service of the Order of Malta (HCSOM). The complete list of 300 FeTe municipalities can be found in Annex 3 of Government Decision 1057/2021 (19.II.). In total, 171 control locations were selected with a respected population of 207,375 people in 2022 (Supplementary Tables 1 – Control Locations).
Population
To get a relevant and most up to date picture of the current medical state of the Programme area, demographic and socioeconomic factors were compared, to demonstrate the difficulties of the healthcare situation in the examined area. The demographic values (age distribution, crude live birth rate, crude mortality rate, educational level, proportion of the roma population) of the Programme were compared to the national averages, based on the 2022 Hungarian census database. For age distribution, according to the Hungarian census, three categories were applied namely, 0–20 years old; 20–60 years old and above 60 years old. The crude live birth rate, the crude mortality rate and the natural increase were analysed as well as the average life expectancy of the populations. To assess the complex socio-economic situation, the proportion of the roma population to the whole population just like the educational status of the residents in the Programme were examined.
Description of health care coverage
Of the 6342 general practices with designated service area in the country, 819 GPs (12,91%) are permanently vacated, meaning more than 6 months of absence of permanent medical staff. At the time of research, from the 32 GP practices in the Programme settlements, 15 (46.88%) practices were vacated and none of these practices were supplemented with permanent GP services. The national average for residents per doctor was 1,488.65 in 2022. The average in the Programme areas was considerably higher, namely 3,010 residents per doctor, indicating a severe shortage of healthcare providers. The standardized prevalence of GP-patient encounters in the Programme as a whole and in all individual districts were significantly higher than the national average (Table 1).
The proportion of people in the Programme who encountered outpatient specialist care with GP referrals (1.40%) was not significantly different from either the national average (1.68%) nor the control area (1.45%). The lowest rate of people attending outpatient specialist care with a GP referral was 1.09% and the highest value was 1,54% in the intervention area. All the districts were under the national thresholds, but only one (Litke) showed significantly lower referral rates than the national average (Supplementary Tables 2 – Difference in outpatient specialist attendance).
The mobile healthcare service centre
In the Programme, healthcare services are delivered through specialized Mobile Healthcare Service Centers (MHSCs). These MHSCs are converted from Fiat Ducato Maxi 250™ or 250™ (L3/H2; Fiat™, Torino, Italy) vehicles (Fig. 2A ,B). Each vehicle was equipped with power aggregators, ensuring a stable power supply under all conditions, compatible with both 230 V and industrial power outlets (16/32 A). Due to the limited access to internet services in the settlements, two different internet providers were involved, namely Vodafone Group plc (Newbury, United Kingdom) and Telekom Hungary (Budapest, Hungary), with a Wi-Fi router (MikroTik™ HAP AC Lit; Riga, Latvia) optimized to connect to the strongest bandwidth vary from 4 Mb/s to 10 Mb/s on average. However, the available bandwidth varied widely across different locations. The lowest recorded download speed was 0.9 Mb/s, while the highest was 86.2 Mb/s. Upload speeds ranged from a minimum of 0.08 Mbit/s to a maximum of 66.3 Mb/s. The MHSCs are outfitted with telemedicine and POCT instruments to support screening and telespecialist consultations (Fig. 2C). This MHCSs enable to perform two levels of telemedical services which are general, basic medical support by GPs and specialized medical consultation. The general medical support provides an physical examination performed by a nurse and further telemedical support by GPs. The next level of care is the implementation of specialists with specialized medical knowledge in a given discipline, e.g. cardiologists, dermatologists, pulmonologists and endocrinologists assist patients in the context of telecare. Based on the results of initial physical examination, the nurse and the GP decide if a specialist should be involved to the care. The visual assessments were conducted by a Firefly™ (Firefly Global, Belmont, Massachusetts, United States) camera system, which includes an otoscope, dermatoscope, and general camera. As point-of-care tests, an Aidan QuickRead Go™ (Aidan, Espoo, Finland) has been installed for rapid c-reactive protein (CRP), Streptococcus-A, and HgbA1C measurements; a Docureader 2™ (77 Elektronika Ltd., Budapest, Hungary) for urine examinations (glucose, ketones, specific gravity, blood, pH, protein, nitrites, bilirubin, urobilinogen, leukocytes); Roche CoaguCheck™ (Roche, Basel, Switzerland) for prothrombin time test (INR) and a Norma™ for blood testing (complete blood count, hemoglobin, hematocrit, white blood cell count, platelet count). MESI™ (MESI Ltd., Ljubljana, Slovenia) system was implemented for ECG testing, spirometry, and ankle-brachial index measurements. Body temperature was measured with an iHealth™ (Sunnyvale, California, United States) thermometer, and fast glucose level screening was conducted by a D-cont™ (77 Elektronika Ltd., Budapest, Hungary) blood sugar testing device. For screening of heart and lung sounds, a digital phonendoscope was used: EKO Duo™ (Emeryville, California, United States) and Thinkabs™ (Centennial, Colorado, United States). The audiovisual connection between the patient, healthcare worker, and telespecialist doctors was supported by a MacBook Pro™ (Apple Inc., Cupertino, California, United States) and a Sandberg™ (Sandberg, Birkerød, Denmark) camera. Patient management were supported by a web-based software solution, NetDoktor™ (Dericom Ltd; Budapest, Hungary). (Fig. 2C) Overall, 12 MHSCs were involved in the Programme.
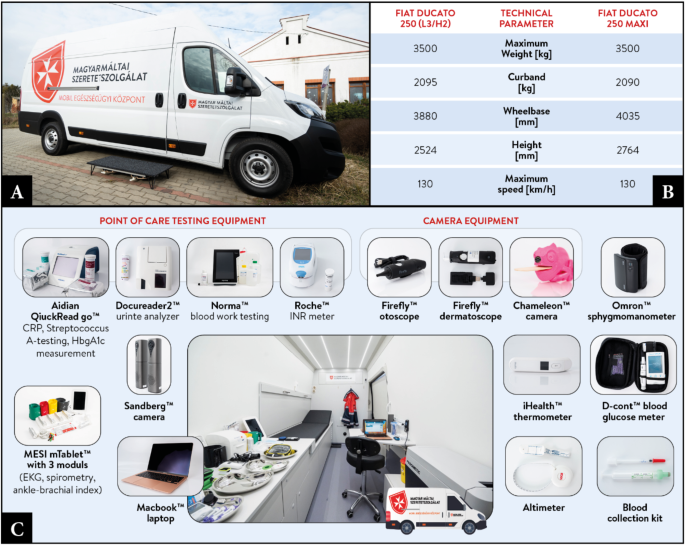
Mobile healthcare service center, developed and constructed in the programme. (A) Fiat Ducato 250 Max MHSC (B) main technical parameters of the vehicles (C) telemedicine and POCT devices applied on the MHSC.
Telemedicine intervention
The telemedicine intervention provided a wide range of healthcare services tailored to the needs of rural populations. Primary prevention was facilitated through community-based health education events known as “Health Forums,” which were regularly held in all serviced settlements. Secondary prevention focused on cardiometabolic screening programs, enabling early detection of chronic conditions. In addition to preventive care, the system offered acute care for a limited range of indications, although certain conditions, such as abdominal complaints, posed challenges due to the limitations of remote diagnostics. Long-term follow-up was available for chronic disease management, ensuring continuity of care. The intervention also optimized patient pathways, facilitating diagnostic coordination and referral efficiency. Furthermore, distinct ultrasound services were integrated, enhancing diagnostic capabilities. These services were available to all patients, regardless of age, from infancy to elderly individuals.
The system relied on a specialized medical software platform designed specifically for Hungarian healthcare providers. This was supplemented by videoconferencing software for teleconsultations with specialists and proprietary diagnostic software (e.g., MESI for ECG, spirometry, and ankle-brachial index measurements). Database management and administrative tasks were supported by Microsoft products, ensuring seamless data handling.
Healthcare professionals involved in the intervention underwent structured training programs. Nurses participated in regular training sessions, with new employees undergoing a three-month training period before full integration to the program. Additionally, a dedicated training day was scheduled at least once per month for continuous skill development. Medical doctors were also trained to use telemedicine diagnostic tools before joining the team and were required to attend webinars at least twice a month to stay updated on best practices.
Cost analysis
The publicly funded single insurer healthcare system of Hungary provided the opportunity to use publicly available databases to assess the per capita spending in primary care in various settings. As the publicly funded Hungarian primary healthcare is financed using a flat rate mostly based on the size and age constitution of the practice population, knowing the size and type of the practices, the typical spending for the various practice types could be determined. The payments for all healthcare providers are published monthly by the National Health Insurance Fund (Nemzeti Egeszsegbiztositasi Alapkezelo, NEAK). In a separate database, the NEAK also publishes monthly status of all primary care practices including location, population size, type (urban adult, urban pediatric or rural mixed practices) and status (vacant or occupied). Dor the calculations, these two databases were matched. In order to maintain the consistency of the calculations, financial data from providers operating multiple primary care practices with different status had to be excluded, as the financial data were published at the provider and not at the individual practice level (data for 173 of the total 6342 practices were excluded for this reason). If a single provider operated multiple practices with the same status, single practice spending was assumed as the average per praxis spending of the provider. Per capita monthly spending in primary care then was calculated for every practice in the exam group using the individual practices’ population data as a denominator.
Since initial data was given in HUF, the calculations were made in HUF as well. The costs were in HUF, and to reflect this, the calculations were also made in HUF. However, to ease the understanding, the final results are presented in US dollar terms, converted on mid-rate (published by Hungarian National Bank) and 350.20 was used for the USD/HUF currency pair.
User feedback questionnaire
To evaluate the experience and satisfaction of patients and doctors with the telemedicine system of the Programme, a structured user feedback questionnaire was created by the research team. The questionnaire was designed to capture various aspects of the user experience, and it contained closed–ended questions, which utilized Likert scales to measure satisfaction, likelihood of returning, and likelihood of recommending the service to others.
The questionnaire was distributed to patients following their telemedicine consultation, and responses were collected either electronically or via paper forms depending on patient preference or accessibility. A total of 206 out of 1,889 patients completed the questionnaire. (The translated patient questionnaire can be found in Supplementary Material 1 – Patient feedback questionnaire) In parallel, a separate questionnaire was designed for the healthcare providers who participated in the telemedicine intervention. This questionnaire aimed to assess their experiences with the telemedicine system, the perceived quality of care delivered through this medium, and their overall satisfaction with the telemedicine workflow. The doctor questionnaire included questions on the frequency of use, the perceived quality of telemedicine care compared to in–person care, and their willingness to continue using telemedicine in the future. A total of 17 out of 24 doctors filled out the questionnaire. (The translated doctor questionnaire can be found in Supplementary Material 2 – Doctor feedback questionnaire)
Data and statistical analysis
The demographic and socio–economic data were obtained from the Central Statistical Office census data for 2022, including age, gender, educational attainment, income level, and economic activity, while the health data was provided by NEAK. A register of all patients who used a healthcare service provided by the intervention program was created, including sociodemographic data, economic activity, participation in public health screenings, and the purpose of attendance. Patients without a social security number in the register were excluded from the analysis. Statistical analyses were conducted using Jamovi 2.3.28 software. For descriptive statistics, we calculated the number of cases (n), proportions (%), and corresponding 95% confidence intervals for the indicator values. Differences between the program and national values/ratios were assessed using the Mann–Whitney U test due to non–normal distribution and lack of homogeneity in the sample, as indicated by pre–testing (Levene’s test). The raw indicator values were calculated as percentages (%). After adjusting for age, sex, and eligibility for public health care, we calculated the standardized indicator values for the baseline period, December 2021. Standardized prevalence ratios were used to characterize the indicators, accounting for the effects of patient age, sex, and eligibility for public health care as proxy variables for socioeconomic status. Additionally, we determined the 95% confidence intervals of the standardized prevalence coefficients, which were used to assess the variability of quantifiable indicator values in GP districts in the program area compared to those in the national or control areas. Mortality tables were used to estimate life expectancy at birth. Mortality and life expectancy data were derived from NEAK’s aggregated mortality tables, using the Chiang method for settlement-level life expectancy calculations37. When carrying out the financial analysis the average per capita spending with standard deviation was calculated for the subpopulations of practices of various types and vacancy status using Microsoft Excel. Data are presented as mean ± SEM (Standard Error of the Mean).
The analysis was conducted using Jamovi 2.3.28.
Descriptive statistics included case counts (n), proportions (%), and 95% confidence intervals.
Regarding subgroup analyses, stratifications based on age, gender, and district-level differences were examined in key outcome measures. These analyses provided additional insights into variations in healthcare utilization and service accessibility within the intervention areas.
Regarding data collection challenges, missing data and technological limitations in certain rural areas were mitigated through standardized data collection procedures and validation mechanisms. In cases where healthcare utilization data were incomplete, cross-referencing with census-based population statistics allowed for improved data accuracy.
Data handling and ethical considerations
The study was approved by the Hungarian Medical Research Council (ETT–TUKEB; BM/9240– 3 /2023). All the patient data were anonymized before analysis, and written consent has been obtained by the participants. All methods were carried out in accordance with relevant regulations and the study was conducted in accordance with the Helsinki Declaration.
The ethical principles and data privacy measures applied in this telemedicine intervention align with standard medical practice and adhere to national and EU data protection regulations, including GDPR (General Data Protection Regulation). All patient data, including electronic health records and telemedicine consultation details, are encrypted and securely stored to prevent unauthorized access. The videoconferencing communication channel used for remote consultations is end-to-end encrypted, ensuring the confidentiality of patient-doctor interactions.
Additionally, all informed consent statements are signed by both the patient and the attending nurse, and they are systematically collected and stored to ensure compliance with data protection regulations.

