Nurses and midwives who lead on the development and roll out of emergent technology in the NHS have discussed what they think the future of digitally-enabled nursing will look like.
At Digital Health Rewired 2025, a conference held earlier this week in Birmingham, chief nursing information officers (CNIOs) and other digital nurses and midwives gathered to celebrate progress so far and discuss which new technologies could help their patients.
“We need to educate all of us, me included, about what AI can do”
Helen Balsdon
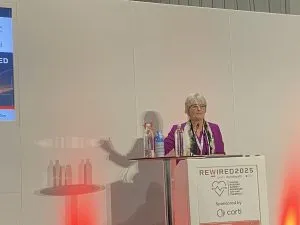
Among those speaking at the conference was NHS England national CNIO Helen Balsdon.
In a keynote speech delivered to the conference, Ms Balsdon said further tech could “make a difference” to nursing, and affirmed her belief in the potential of artificial intelligence (AI) to help the profession.
AI refers to a range of different technologies, including – but not limited to – generative tools like ChatGPT, machine and algorithmic learning technology based on data sets and automated diagnostic tools.
However, Ms Balsdon told Nursing Times that she felt one particular sub-set of AI, ambient voice technology (AVT), excited her the most.
AVT is able to monitor what a person is saying, or a conversation between mulitple people, in the background.
It can then use a mixture of speech recognition and large-language model (LLM) AI to create a summary or interpret this conversation.
In healthcare, AVT has been trialled, particualrly in the US, to quickly create clinical notes based on conversations between clinicians and patients.
However, concerns exist about privacy implications of the software and about trust in the systems.
Ms Balsdon suggested that, if it proves effective, AVT could be used by nurses in both the community and hospitals.
“I think that’s where the opportunity is,” she said. “I would love to explore it more.”

Helen Balsdon
In her conference presentation, Ms Balsdon said AI, and in particular AVT, “has got the potential”, but that it “needs to be adopted well”.
She called on the nursing and midwifery professions to help create an evidence base that could help decide how, or if, these technologies were used.
“It should be for all clinical professions, not just the one. We’ve got no case studies across the world, that I can find, for anything other than our medical colleagues,” she said.
“We need to look at it and be really creative about how [it is] working.”
Ms Balsdon added: “We need to educate all of us, me included, about what AI can do, what the potential is. There’s a lot of hype, we’ve got to build those foundations.”
She pointed to ongoing work at NHS England to build training and advice on AI into the NHS Futures platform, which allows NHS staff from different areas to share learning and ideas.
In order for AI to work, however, Ms Balsdon stressed that CNIOs, and other digital nurses, must help build the foundations: better data, a more digitally-informed workforce and roll outs that are patient focused.
Ms Balsdon appeared on a panel at Digital Health Rewired alongside national chief midwifery information officer (CMIO) Jules Gudgeon, national chief pharmacy and medicines information officer Rahul Singal and Prabha Vijayakumar, national chief allied health professionals information officer.
This panel was chaired by University Hospitals of Leicester NHS Trust CNIO Hayley Grafton.
Ms Grafton asked the panel what leading digital nurses and midwives can do to ensure the NHS, and the professions, were ready to make the most out of emergent technology and to “crest the wave”.
Ms Balsdon said: “I think we’ve got to build really firm foundations… we’ve got to build those, and we have to use our voice.”
She later added: “The [electronic patient record] is just the starting place. There’s more technology coming, and technology… could add value to what we do.
“But we need the core foundations equip everybody with the knowledge and skills, use our digital leadership and make sure we are really guiding our executive leadership to make some of those decisions.
“But it’s important, especially in the next few years, when money is tight, [that] we actually use the community to make some of the decisions about priorities.
“The reality is we’re not going to be able to do everything, so what are our choices and how are they going to get us there? We need to keep that end goal in mind, because we’ve got to make incremental change and take everybody on that journey.”
CMIO Ms Gudgeon, during the same panel session, said the “appetite is there” for utilising technology to improve midwifery care.
She pointed to the upcoming launch of a national digital self-referral service for pregnant women seeking maternity care as an example of foundational improvements that are being made in this sphere.
Ms Gudgeon said: “It’s something so simple… why did we never do that before?
“There are examples of things like that all over, and that’s what going from analogue to digital really means.”
The CMIO also called for more collaboration between digital nurses and midwives: “We’ve got so much to learn from one another.
“It’s wrong if we isolate ourselves, and that’s how we can take this forward. We have to be stronger together.”
Ms Gudgeon and Ms Balsdon also called for further improvements to career pathways for digital nurses, although acknowledged that progress had already been made.
Digital innovations in community nursing also got a spotlight at Rewired.
Dr Crystal Oldman, outgoing chief executive of the Queen’s Institute for Community Nursing (QICN, formerly the Queen’s Nursing Institute), told the conference that the workforce she represents was keen to embrace technology to improve care, but that it must be done in a way that makes work easier, not more complex.
Crystal Oldman
She pointed to one example from a recent QICN report of a community nurse who had 44 different logins for different systems they were being asked to use.
Dr Oldman said: “[The report showed] nurses in the community being very positive about engagement with digital technology, high levels of digital literacy, high levels of enthusiasm about the potential [it has] to support patients…
“However, there was poor access and poor experience of digital applications.”
Caroline Palmer, a Queen’s Nurse and clinical lead for digital health transformation at Leicester Partnership NHS Trust, told the conference about a digital platform she helped develop at her organisation that allowed patients at home to speak directly to clinicians.
The platform, ChatHealth, is a confidential messaging service that connects patients to the relevant healthcare workers.
Ms Palmer said the technology had helped new mothers feel less isolated by easily connecting them to health visitors.
“Access to healthcare should be as easy as access to everything else that we use in life,” she said, explaining how the platform was developed in Leicester.

Caroline Palmer
“So, we chose to communicate with service users… via messaging, but we wanted it to be safe and secure and fit for kind of purpose within the NHS.
“We looked at off-the-shelf products where we couldn’t find anything, and so that’s why we created our own platform.”
Since its rollout in Leicestershire, the platform is now used by more than 80 NHS organisations, Ms Palmer said.
She told the conference that she felt it was a good example of how technology, with input from nurses, could help improve access to healthcare.
More on digital nursing

