(The opinions and views expressed in the commentaries and letters to the Editor of The Somerville Times belong solely to the authors and do not reflect the views or opinions of The Somerville Times, its staff or publishers)

By Senator Patricia D. Jehlen
I am Senate chair of the Labor and Workforce Development Committee and the Committee on Elder Affairs. Each of those committees produced a major bill this session which passed the legislature and was signed, or is about to be signed, into law.
In an earlier newsletter, I wrote about the Labor Committee’s wage transparency law.
The second bill, about long-term care facilities for older people and people with disabilities, hadn’t passed by the time formal sessions ended on July 31. In the informal sessions that continue after that, any one legislator could object and stop the bill. Despite that, I am happy and relieved to be able to report that the long-term care bill passed the legislature last Thursday.
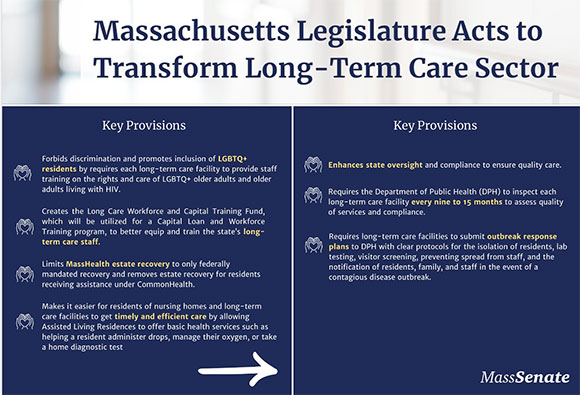
An Act to improve quality and oversight of long-term care strengthens the Commonwealth’s oversight of nursing homes, provides critical anti-discrimination protections for LGBTQ+ nursing home residents, and permanently allows assisted living residences to offer basic health services. And a lot more.
The Globe praised the bill’s passage in an editorial, “A step toward ending nursing home horror stories.” The Herald printed part of an AP story, “Nursing home oversight would be tightened.” The Disability Policy Consortium wrote, “DPC is thrilled that the Long Term Care Bill (H.5033) has passed both the House and Senate. This bill contains many items that will improve the lives of people with disabilities in Massachusetts, from strengthening infection control standards for nursing homes to prevent the kinds of mass outbreaks we saw in 2020, to stricter suitability reviews and more scrutiny of Private Equity’s impact on the sector.” The Mass. Guardianship Policy Institute wrote, “This is a huge accomplishment, one that you have worked on for years, to address a long-term care crisis laid bare by Covid,” mentioning several components of the bill.
This is a long newsletter because it’s a long (66 page) and complicated bill. It now includes several other bills that many of us have worked hard on for many years. Like the bill, this newsletter is long, including information on nursing homes, assisted living residences, LGBTQI rights, pooled trusts, prior authorization, estate recovery and more. You can skim if only some parts interest you.
NURSING HOMES: FUNDING AND ACCOUNTABILITY
Many people have called and written to tell about neglect and mistreatment of themselves or their relatives in nursing homes. There have been many investigations and media reports of these problems and of sudden closures.

Kay Lazar’s Globe reports about overuse of anti-psychotic drugs, poor care, and expansion of for-profit chains shocked readers starting in 2010. Most recently there’s been a lot of regional coverage about homes in South Hadley and Northampton. Jack Styler of The Provincetown Independent has done deep reporting on the poor care as well as the finances of the for-profit Advinia nursing home, the only one within 30 miles. (Sadly, that 2-star facility in Medicare ratings was at least 3 stars in 2019, as shown in the chart at the right from the Nursing Facility Task Force.)
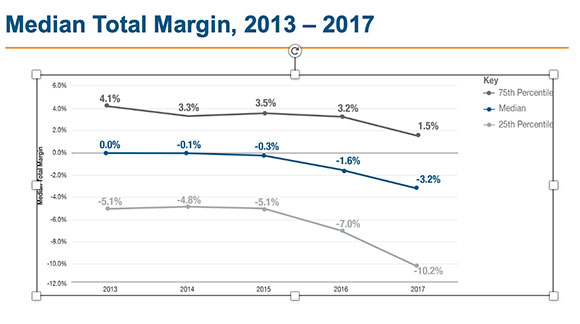
At the same time, nursing homes report operating losses and many have closed.
We all have focused on the disaster of Steward hospitals. The trend toward for-profit companies gaining a larger and larger share of nursing homes, home care agencies, and hospices is equally troubling. Nursing homes too often extract the value from these institutions by cutting staff, not paying staff and other bills, selling the buildings to related Real Estate Investment Trusts and paying exorbitant fees and rents, and then closing or being closed. Hospices, as John Oliver reported
I wrote about hearings on the effect of increasing dominance by private equity here. As of 2020, 70% of Massachusetts nursing homes were owned by for-profit companies.
Meanwhile, in just 13 years, MA lost 23% of its nursing home beds, while the number of older adults is growing.
I wondered why nursing homes always seemed to be underfunded and yet were being rapidly bought by large for-profit companies.
In 2019, the Nursing Facility Task Force brought together a wide range of stakeholders to examine the related nursing home problems of low occupancy, closures and inadequate payments.
The Task Force made recommendations to ensure the survival of essential, quality homes with regional availability, while ensuring that those that closed were those with low census and low quality.
We issued the report in February 2020. But when the pandemic hit, we all focused on the immediate crisis, in which up to 1/4 of nursing home residents died. The pandemic revealed starkly that nursing homes were unprepared to stop the spread of disease. Many of us knew people who died. Even nursing homes with high ratings lost many residents and workers.
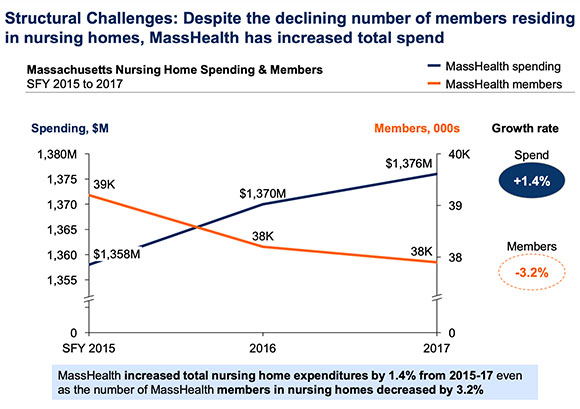
Following the report, the legislature has increased funding and added spending accountability to ensure money gets to the workers. The Baker and Healey administrations have worked to keep essential nursing homes afloat while ensuring that those that closed were low quality and less regionally important.
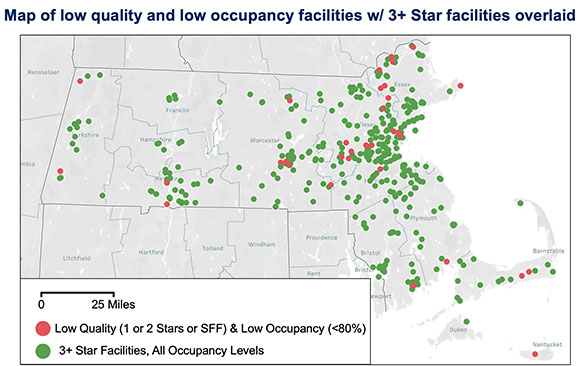
Already, 100% of the 31 closures since the Task Force have had only 1 or 2 stars. 40% of the closures in 2022 were in the lowest 5% on Department of Public Health (DPH) surveys. But more reforms are needed, as shown for example in this Disability Law Center report on a Worcester facility.
Our bill will increase capital funding for nursing homes to create training and career ladders and to adjust their buildings to different needs. And it will require more realistic updating of the base rate every 2 years.
It will expand DPH tools:
More oversight, including suitability standards. Those standards will allow DPH to limit, restrict, suspend, or revoke a license; or deny a license or license transfer. They can also appoint temporary facility managers for troubled facilities.
Increase civil penalties the Attorney General can seek by 10 times (for example, increase to $250,000 for a death).
Increase by 10 times fines DPH can levy for noncompliance with regulations. Right now, the maximum fine is $50/a day, the same as the minimum fine for a speeding ticket.
Require regular inspections and outbreak response plans
Require clear standards for special care units.
COMMON SENSE CARE IN ASSISTED LIVING
This bill incorporates my assisted living bill: it will make permanent the temporary allowance for Assisted Living Residences (ALRs) to offer basic health services. ALRs are certified by the Executive Office of Elder Affairs, not DPH, and are considered non-medical facilities. They each have a nurse on staff. But those nurses weren’t allowed to do simple things like administering eyedrops or insulin injections. So when someone needed those things – things most people can do for themselves or family members – they had to hire another nurse or get family members to come in and help them. If it was something like insulin, which would be more permanent, they usually had to move to a nursing home at more expense to themselves and eventually the state, and suffer the disorientation and trauma of moving.
During the pandemic, there has been a temporary allowance for ALR nurses to provide these services. There have been no cases of bad results. But that allowance expires next March.
This bill continues the option for ALRs to offer those services. The bill also requires more disclosure of ownership, and provides for fines of $500 a day in cases of failure to follow regulations.
SMALL HOUSE NURSING HOMES
One of my other bills we’ve worked on for years is incorporated in this one. It provides for regulations to create small house nursing homes, which serve 14 or fewer residents in more homelike environments. Small house nursing homes had far fewer cases of COVID.
LGBTQI BILL OF RIGHTS
Another of my bills incorporated in this one is the LGBTQI bill of rights for nursing home residents, banning discrimination and requiring training of staff. This came out of the work by the LGBTQ Aging Commission. I vividly remember testimony at one of the commission hearings. A family in Western Mass could no longer care for their transgender aunt. They could not find a single nursing home that would admit her. Finally, they found one. And that one ironically put her in a converted closet. That reminded me of the film, Gen Silent, about how people, faced with caregivers who might judge them, went back in the closet when they needed care. (You can watch Gen Silent on Kanopy through your local public library.)
SPECIAL NEEDS POOLED TRUSTS
Another of my bills incorporated here addresses special needs pooled trusts. A pooled trust contains the assets of many individuals that are held or “pooled” in separate trust accounts. People with disabilities under 65 can transfer resources to a special needs trust to reduce their assets to $2000 so they can qualify for Mass Health. That money can be used for needs like home care, home adaptations, personal items, and assisted living expenses. For 30 years, until this spring, MassHealth allowed older people with disabilities to establish and use pooled trusts, and we need to restore that option. Any unexpended money from the trust is sent to MassHealth for their benefits when the person dies. Millions of dollars are reimbursed to Mass Health every year.
PRIOR AUTHORIZATION FOR TRANSFER FROM HOSPITALS
In June, there were 1792 patients stuck in hospitals, awaiting discharge to nursing homes, home care or other care. Some are waiting because there’s not enough staff in the nursing home or home care agency they’re going to. But many are waiting for prior authorization from their insurance company.
There will now be a uniform prior authorization form. And insurers must approve or deny prior authorization for transfer of patients from hospitals to nursing homes within one business day. This will prevent patients from being stuck in hospitals waiting for insurance approval, but it doesn’t mean there will be enough staff in either nursing homes or home care.
Mass Hospital Association wrote: “We are hopeful that this legislation can help free up some of the 1,700 hospital beds occupied by patients in need of post-acute care services.”
ESTATE RECOVERY LIMITS
Finally, the bill limits estate recovery from Medicaid recipients to spending to the federal requirement of recovery of nursing home expenses. MassHealth has gone farther, recovering funds spent for any medical care after the person turns 55. A bill by Rep. Christine Barber and Senator Jo Comerford, incorporated here, will prevent family members from losing the homes where they had cared for their disabled relatives, and prevent generational impoverishment.
Disability Policy Consortium adds: “The bill also prohibits estate recovery for adults in the CommonHealth program and for personal care attendant services, both of which enable people with disabilities to live, work, and thrive in the community.”
PLANNING FOR NEXT STEPS
The bill creates task forces and studies to inform our next steps in improving long term care. These groups would examine issues like hospital throughput, MassHealth Long Term Care eligibility, Medicare ACOs, rest homes, Continuing Care Retirement Communities, and further ALR reforms. We need to strengthen all the pieces of the entire care continuum, from home care to adult day health to rest homes to assisted living to nursing homes.
STILL URGENTLY NEEDED
This is very important, comprehensive and long-needed legislation. But there’s much more we need to do.
We need the administration to explore a frail elder waiver to enable development of affordable assisted living, although a provision in the Housing Bond Bill may do similar work.
We need to pass the bill requiring home care agencies to be licensed. It’s currently before the House.
We need to make permanent the provision for holding beds for nursing home residents who leave for medical care instead of making it depend on annual budgets as it has for decades.
We need to increase the personal needs allowance, which is the amount nursing home residents can keep from their social security to pay for things like haircuts and birthday cards. The allowance of $72.80 a month has not been raised for over 30 years.
We need to make sure DPH has adequate resources and the will to use the tools we are giving them to ensure quality care.
The Elder Affairs secretary should be restored to the cabinet. Elder Affairs is now the only executive office whose secretary is not in the cabinet. The role should be given that recognition and the responsibility to bring the intersecting needs of older adults into all discussions.
And we need to continue to address the workforce crisis.

