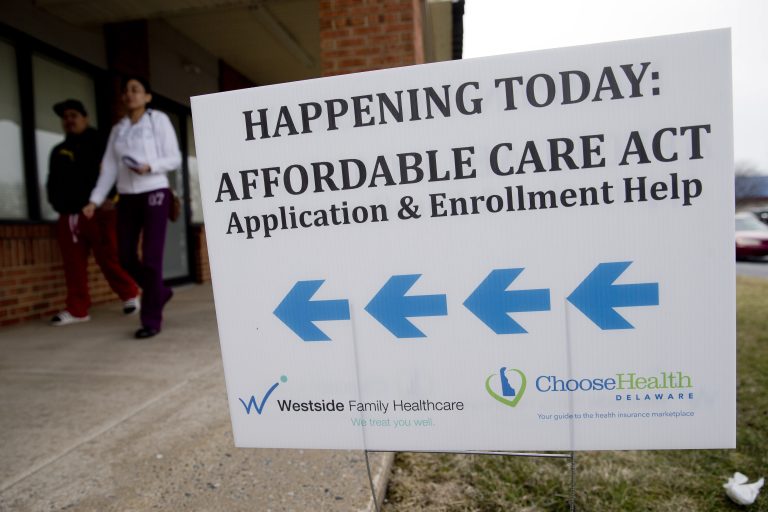
The Trump administration issued the first major set of changes proposed to the Affordable Care Act on Monday, when federal officials said they intended to crack down on program fraud. Policy experts said it would make it difficult for consumers to register for compensation, and could reduce enrollment.
Details were released Monday after a draft press release was previously incorrectly posted.
Approximately 24 million Americans signed up for an insurance plan sold at the ACA, commonly known as Obamacare in 2025. The Biden administration has achieved record-breaking registration levels after increasing premium subsidies for many low-income people. It also made it easier for some very low-income people to sign up anytime, at any time, rather than waiting for their registration period each fall. However, the program suffered from fraudulent registrations last year, generating roughly 274,000 consumer complaints by August. It focuses on fraud insurance agents and other bad actors, and on the Centers for Medicare & Medicaid Services.
The Trump administration said in a statement Monday that the new regulations “contain important and necessary steps to promote a stable and affordable health insurance market and protect people who are registered in market coverage without knowledge or consent, and to ensure that ACA has financial support for taxpayer dollars only for those seeking support.”
However, policy experts said the change would place a burden on new documents that could hinder registration.
“Under this flag that attempts to crack down on the bad behavior of some insurance brokers, they are punished by consumers, especially low-income consumers, with more cumbersome requirements and more restrictions on access to coverage.”
Among other new requirements, consumers will need to provide more information to prove their special registration period and eligibility for premium subsidies at the time of registration. Additionally, regulations will shorten the annual registration period to one month. It then touches on social issues and limits the eligibility of “dreamers.” This is the nickname for the immigrants of the country who brought here as a child based on a never-passed proposal called the Dream Act.
This proposal would eliminate annual opportunities for special enrollment periods for people with very low incomes. However, you can also set new requirements for the remaining special registration period. This allows people to sign up after major life events, such as losing work-based coverage, divorce, marriage, or moving when income changes. When applying under these special circumstances, they must provide evidence of their eligibility.
Those who automatically register for Zero Premium Plans during their regular enrollment period will be charged a small monthly payment until they review or update their information.
According to the proposal, the ACA market will need to seek additional data from consumers, including self-employed and gig workers, which estimate income for next year but do not have tax return data filed with the IRS the previous year.
The Biden administration made changes last year to reduce fraudulent registrations, including requiring three-way calls between insurance brokers, their clients, and the federal insurance market, Healthcare.gov when certain sign-up or coverage changes were made.
Some of the Trump administration's proposed changes could help warn certain consumers that they are registered with an ACA plan without their knowledge. For example, even the cheapest plans require you to receive a small monthly premium invoice.
However, Cynthia Cox, vice president and director of KFF ACA's program, a health information nonprofit organization that includes KFF Health News, said: “Some of them may be protecting subscribers who have been fraudulently signed up or they may not realize they are still signed up.”
Still, if you can't document the expected income changes, it can prove difficult for some people. “They may have a legitimate claim, but they have a hard time demonstrating it,” Cox said.
The annual registration period ends on December 15th, one month earlier than this year. The specified period is when most people sign up and aim to prevent people from waiting until they get sick.
Trump's proposal also touches on social issues.
It would reverse Biden administration policies that allow dreamers to qualify for granted ACA compensation. The decision is already subject to court challenges brought by 19 states seeking to overturn it.
Also, under Trump's proposal, gender-maintaining care is not considered part of the “intrinsic health benefits” that all plans must cover.
According to the FAQ accompanying the initial press release of the proposed regulations, the provisions “may lead to increased out-of-pocket costs for individuals requiring sexual correction services.
As a proposed rule, the measure currently faces a period of public comment and potential revisions.
“We've seen a lot of experience in the health policy and law,” said Katie Keith, director of Georgetown University's Center for Health Policy and Law. “The question is how much it will apply to 2025 and 2026.”
The FAQ acknowledged that some of the proposed changes, including termination of annual enrolment for very low-income people, could “increase the administrative burden on consumers associated with the registration and verification process or prevent eligible low-income people from registering.
However, “We believe that increasing program integrity and reducing inappropriate enrollment will outweigh coverage access.”
Some lawmakers and conservative groups point to concerns about fraudulent registration and the role of ACA grants or registration periods in promoting the issue.
For example, the right-leaning Paragon Health Institute released a report in June that it called for an expansion of the Biden administration, especially in a special registration period, to help lower-income earners turn around.
“There was a considerable amount of fraud and waste on the ACA exchange, and the Biden administration pursued all registration cost strategies and was tolerant of waste, fraud and abuse,” said Brian Blaze, president of the current Paragon Health Institute within the Trump administration and the first president of the influential President Trump. “Obviously, there's a different approach to protecting legitimate enrollees and taxpayers.”
jappleby@kff.org, @julie_appleby