Alonso R, Perez de Isla L, Muñiz-Grijalvo O, Diaz-Diaz JL, Mata P. Familial hypercholesterolaemia diagnosis and management. Eur Cardiol Rev. 2018;13:14–20. https://doi.org/10.15420/ecr.2018:10:2.
Google Scholar
Dheensa S, Fenwick A, Shkedi-Rafid S, Crawford G, Lucassen A. Health-care professionals’ responsibility to patients’ relatives in genetic medicine: a systematic review and synthesis of empirical research. Genet Med. 2016;18:290–301. https://doi.org/10.1038/gim.2015.72.
Google Scholar
Menko FH, Ter Stege JA, van der Kolk LE, Jeanson KN, Schats W, Moha DA, et al. The uptake of presymptomatic genetic testing in hereditary breast-ovarian cancer and Lynch syndrome: a systematic review of the literature and implications for clinical practice. Fam Cancer. 2019;18:127–35. https://doi.org/10.1007/s10689-018-0089-z.
Google Scholar
Parker M, Lucassen A. Using a genetic test result in the care of family members: how does the duty of confidentiality apply? Eur J Hum Genet. 2018;26:955–9. https://doi.org/10.1038/s41431-018-0138-y.
Google Scholar
Frey MK, Ahsan MD, Bergeron H, Lin J, Li X, Fowlkes RK, et al. Cascade testing for hereditary cancer syndromes: should we move toward direct relative contact? a systematic review and meta-analysis. J Clin Oncol: J Am Soc Clin Oncol. 2022;40:4129–43. https://doi.org/10.1200/JCO.22.00303.
Google Scholar
Trevisan L, Godino L, Battistuzzi L, Innella G, Luppi E, Buzzatti G, et al. Cascade testing in Italian Hereditary Breast Ovarian Cancer families: a missed opportunity for cancer prevention? Fam cancer. 2024;23:197–207. https://doi.org/10.1007/s10689-023-00349-w.
Google Scholar
Daly MB, Montgomery S, Bingler R, Ruth K. Communicating genetic test results within the family: Is it lost in translation? A survey of relatives in the randomized six-step study. Fam Cancer. 2016;15:697–706. https://doi.org/10.1007/s10689-016-9889-1.
Google Scholar
Srinivasan S, Won NY, Dotson WD, Wright ST, Roberts MC. Barriers and facilitators for cascade testing in genetic conditions: a systematic review. Eur J Hum Genet Eur J Hum Genet. 2020;28:1631–44. https://doi.org/10.1038/s41431-020-00725-5.
Google Scholar
Austin J. Re‐conceptualizing risk in genetic counseling: implications for clinical practice. J Genet Couns. 2010;19:228–34. https://doi.org/10.1007/s10897-010-9279-z.
Google Scholar
Shah L, Daack‐Hirsch S, Ersig A, Paik A, Ahmad F, Williams J. Family relationships associated with communication and testing for inherited cardiac conditions. West J Nurs Res. 2018;41:1576–601. https://doi.org/10.1177/0193945918817039.
Google Scholar
Wiens M, Wilson B, Honeywell C, Etchegary H. A family genetic risk communication framework: guiding tool development in genetics health services. J Community Genet. 2013;4:233–42. https://doi.org/10.1007/s12687-012-0134-9.
Google Scholar
Dheensa S, Fenwick A, Lucassen A. Is this knowledge mine and nobody else’s? I don’t feel that.’Patient views about consent, confidentiality and information-sharing in genetic medicine. J Med Ethics. 2016;42:174–9. https://doi.org/10.1136/medethics-2015-102781.
Google Scholar
Dheensa S, Lucassen A, Fenwick A. Limitations and pitfalls of using family letters to communicate genetic risk: a qualitative study with patients and healthcare professionals. J Genet Couns. 2018;27:689–701. https://doi.org/10.1007/s10897-017-0164-x.
Google Scholar
Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract: Int J Kuwait Univ Health Sci Cent. 2021;30:17–28. https://doi.org/10.1159/000509119.
Google Scholar
Aktan-Collan K, Haukkala A, Pylvänäinen K, Järvinen HJ, Aaltonen LA, Peltomäki P, et al. Direct contact in inviting high-risk members of hereditary colon cancer families to genetic counselling and DNA testing. J Med Genet. 2007;44:732–8. https://doi.org/10.1136/jmg.2007.051581.
Google Scholar
Henrikson NB, Blasi P, Figueroa Gray M, Tiffany BT, Scrol A, Ralston JD, et al. Patient and family preferences on health system-led direct contact for cascade screening. J Pers Med. 2021;11:538 https://doi.org/10.3390/jpm11060538.
Google Scholar
Tiller J, Nowak K, Boughtwood T, Otlowski M. Privacy implications of contacting the at-risk relatives of patients with medically actionable genetic predisposition, with patient consent: a hypothetical Australian case study. BioTech. 2023;12:45.
Google Scholar
Privacy Amendment (Enhancing Privacy Protection) Act No 24 (2024) (Australia) https://www.legislation.gov.au/C2004A03712/latest/text (accessed on 12 December 2024).
Henrikson, NB, Wagner, JK, Hampel, H, DeVore, C, Shridhar, N, Williams, JL, et al. (2020) What guidance does HIPAA offer to providers considering familial risk notification and cascade genetic testing? J Law Biosci 7. https://doi.org/10.1093/jlb/lsaa071.
Law No. 2021–1017 dated 2 August 2011 (art. 15) Code de la santé publique. L1131-1, JORF, 2021. https://www.legifrance.gouv.fr/codes/section_lc/LEGITEXT000006072665/LEGISCTA000006171009/#LEGISCTA000043895848 (accessed on 12 December 2024).
Lindberg, LJ, Wadt, KA, Therkildsen, C, & Petersen, HV (2024) National Experiences from 30 Years of Provider-Mediated Cascade Testing in Lynch Syndrome Families-The Danish Model. https://doi.org/10.3390/cancers16081577.
Menko FH, Aalfs CM, Henneman L, Stol Y, Wijdenes M, Otten E, et al. Informing family members of individuals with Lynch syndrome: a guideline for clinical geneticists. Fam Cancer. 2013;12:319–24. https://doi.org/10.1007/s10689-013-9636-9.
Google Scholar
Marleen van den Heuvel L, Stemkens D, van Zelst-Stams WAG, Willeboordse F, Christiaans I. How to inform at-risk relatives? Attitudes of 1379 Dutch patients, relatives, and members of the general population. J Genet Couns. 2020;29:786–99. https://doi.org/10.1002/jgc4.1206.
Google Scholar
Dutch Clinical Genetics Society (VKGN) (2019) Richtlijn Informeren van familieleden bij erfelijke aandoeningen. https://www.vkgn.org/files/5911/Richtlijn%20informeren%20van%20familieleden%20bij%20erfelijke%20aandoeningen.pdf (accessed on 10 September 2024).
Duttge G. The right to know and not to know: predictive genetic diagnosis and non-diagnosis. Recent results cancer Res Fortschr der Krebsforsch Prog dans les Rech sur le cancer. 2021;218:67–83. https://doi.org/10.1007/978-3-030-63749-1_6.
Google Scholar
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev public health. 2014;35:29–45. https://doi.org/10.1146/annurev-publhealth-032013-182440.
Google Scholar
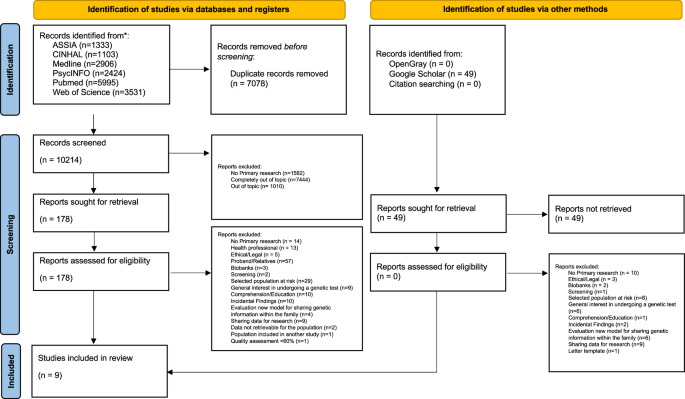
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg (Lond, Engl). 2021;88:105906 https://doi.org/10.1016/j.ijsu.2021.105906.
Google Scholar
Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qualitat Health Res. 2012;22:1435–43. https://doi.org/10.1177/1049732312452938.
Google Scholar
Godino L. How to structure Microsoft Excel documents for systematic reviews. Nurse Res. 2023;31:40–6. https://doi.org/10.7748/nr.2023.e1866.
Google Scholar
Palese A, Mansutti I, Visintini E, Caruzzo D, Moreale R, Longhini J, et al. Framing the time while designing and conducting reviews: A Focused Mapping Review and Synthesis. J Clin Nurs. 2022;31:3523–34. https://doi.org/10.1111/jocn.16180.
Google Scholar
Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. HTA Initiat. 2004;13:1–28. https://doi.org/10.5858/arpa.2020-0217-sa.
Google Scholar
Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. 2020;18:2108–18. https://doi.org/10.11124/JBISRIR-D-19-00169.
Google Scholar
Onwuegbuzie AJ. Effect sizes in qualitative research: a prolegomenon. Qual Quant. 2003;37:393–409. https://doi.org/10.1023/a:1027379223537.
Google Scholar
Hawranek C, Hajdarevic S, Rosén A. A focus group study of perceptions of genetic risk disclosure in members of the public in Sweden: “I’ll Phone the Five Closest Ones, but What Happens to the Other Ten?”. J Pers Med. 2021;11:1191 https://doi.org/10.3390/jpm11111191.
Google Scholar
Andersson A, Hawranek C, Öfverholm A, Ehrencrona H, Grill K, Hajdarevic S, et al. Public support for healthcare-mediated disclosure of hereditary cancer risk information: Results from a population-based survey in Sweden. Hered Cancer Clin Pr. 2020;15:18–30. https://doi.org/10.1186/s13053-020-00151-0.
Google Scholar
Heaton TJ, Chico V. Attitudes towards the sharing of genetic information with at-risk relatives: results of a quantitative survey. Hum Genet. 2016;135:109–20. https://doi.org/10.1007/s00439-015-1612-z.
Google Scholar
Maxwell SJ, Molster CM, Poke SJ, O’Leary P. Communicating familial hypercholesterolemia genetic information within families. Genet Test Mol Biomark. 2009;13:301–6. https://doi.org/10.1089/gtmb.2008.0138.
Google Scholar
Petersen HV, Frederiksen BL, Lautrup CK, Lindberg LJ, Ladelund S, Nilbert M. Unsolicited information letters to increase awareness of Lynch syndrome and familial colorectal cancer: reactions and attitudes. Fam cancer. 2019;18:43–51. https://doi.org/10.1007/s10689-018-0083-5.
Google Scholar
Phillips A, Dewitte I, Debruyne B, Vears DF, Borry P. Disclosure of genetic risk in the family: a survey of the Flemish general population. Eur J Med Genet. 2023;66:104800 https://doi.org/10.1016/j.ejmg.2023.104800.
Google Scholar
Tiller JM, Stott A, Finlay K, Boughtwood T, Madelli EO, Horton A, et al. Direct notification by health professionals of relatives at-risk of genetic conditions (with patient consent): views of the Australian public. Eur J Hum Genet: Eur J Hum Genet. 2024;32:98–108. https://doi.org/10.1038/s41431-023-01395-9.
Google Scholar
Wolff K, Brun W, Kvale G, Nordin K. Confidentiality versus duty to inform-an empirical study on attitudes towards the handling of genetic information. Am J Med Genet Part A. 2007;143A:142–8. https://doi.org/10.1002/ajmg.a.31467.
Google Scholar
Van den Heuvel LM, Smets EMA, van Tintelen JP, Christiaans I. How to inform relatives at risk of hereditary diseases? A mixed-methods systematic review on patient attitudes. J Genet Couns. 2019;28:1042–58. https://doi.org/10.1002/jgc4.1143.
Google Scholar
Zhu X, Smith RA, Parrott RL. Living with a rare health condition: the influence of a support community and public stigma on communication, stress, and available support. J Appl Commun Res. 2017;45:179–98. https://doi.org/10.1080/00909882.2017.1288292.
Google Scholar
Leenen CH, Heijer MD, van der Meer C, Kuipers EJ, van Leerdam ME, Wagner A. Genetic testing for Lynch syndrome: family communication and motivation. Fam cancer. 2016;15:63–73. https://doi.org/10.1007/s10689-015-9842-8.
Google Scholar
Marks D, Thorogood M, Neil SM, Humphries SE, Neil HA. Cascade screening for familial hypercholesterolaemia: implications of a pilot study for national screening programmes. J Med Screen. 2006;13:156–9. https://doi.org/10.1258/096914106778440617.
Google Scholar
Suthers GK, Armstrong J, McCormack J, Trott D. Letting the family know: balancing ethics and effectiveness when notifying relatives about genetic testing for a familial disorder. J Med Genet. 2006;43:665–70. https://doi.org/10.1136/jmg.2005.039172.
Google Scholar
Di Pietro ML, Zaçe D, Orfino A, Di Raimo FR, Poscia A, de Matteis E, et al. Intrafamilial communication of hereditary breast and ovarian cancer genetic information in Italian women: towards a personalised approach. Eur J Hum Genet. 2021;29:250–61. https://doi.org/10.1038/s41431-020-00723-7.
Google Scholar
Weaver M. The double helix: applying an ethic of care to the duty to warn genetic relatives of genetic information. Bioethics. 2016;30:181–7. https://doi.org/10.1111/bioe.12176.
Google Scholar
Mesters I, Ausems M, Eichhorn S, Vasen H. Informing one’s family about genetic testing for hereditary non-polyposis colorectal cancer (HNPCC): a retrospective exploratory study. Fam cancer. 2005;4:163–7. https://doi.org/10.1007/s10689-004-7992-1.
Google Scholar
Stoffel EM, Ford B, Mercado RC, Punglia D, Kohlmann W, Conrad P, et al. Sharing genetic test results in Lynch syndrome: communication with close and distant relatives. Clin Gastroenterol Hepatol : Clin Pr J Am Gastroenterol Assoc. 2008;6:333–8. https://doi.org/10.1016/j.cgh.2007.12.014.
Google Scholar
Hamilton R, Williams JK, Bowers BJ, Calzone K. Life trajectories, genetic testing, and risk reduction decisions in 18-39 year old women at risk for hereditary breast and ovarian cancer. J Genet Couns. 2009;18:147–59. https://doi.org/10.1007/s10897-008-9200-1.
Google Scholar
Geer KP, Ropka ME, Cohn WF, Jones SM, Miesfeldt S. Factors influencing patients’ decisions to decline cancer genetic counseling services. J Genet Couns. 2001;10:25–40. https://doi.org/10.1023/a:1009451213035.
Google Scholar
Godino L, Turchetti D, Jackson L, Hennessy C, Skirton H. Impact of presymptomatic genetic testing on young adults: a systematic review. Eur J Hum Genet. 2016;24:496–503. https://doi.org/10.1038/ejhg.2015.153.
Google Scholar
Godino L, Jackson L, Turchetti D, Hennessy C, Skirton H. Decision making and experiences of young adults undergoing presymptomatic genetic testing for familial cancer: a longitudinal grounded theory study. Eur J Hum Genet. 2018;26:44–53. https://doi.org/10.1038/s41431-017-0030-1.
Google Scholar
Godino L, Turchetti D, Jackson L, Hennessy C, Skirton H. Presymptomatic genetic testing for hereditary cancer in young adults: a survey of young adults and parents. Eur J Hum Genet. 2019;27:291–9. https://doi.org/10.1038/s41431-018-0262-8.
Google Scholar
Godino L, Varesco L, Bruno W, Bruzzone C, Battistuzzi L, Franiuk M, et al. Preferences of Italian patients for return of secondary findings from clinical genome/exome sequencing. J Genet Couns. 2021;30:665–75. https://doi.org/10.1002/jgc4.1350.
Google Scholar
Burke, K, Dawson, L, Hodgkinson, K, Wilson, BJ, Etchegary, H (2024). Exploring family communication preferences in hereditary breast and ovarian cancer and Lynch syndrome: a national Canadian survey. J Community Genet 1-14. https://doi.org/10.1007/s12687-024-00720-z.
Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: a meta-analysis. PloS one. 2017;12:1–13. https://doi.org/10.1371/journal.pone.0170988.
Google Scholar
LePoire E, Basu B, Walker L, Bowen DJ. What do people think about genetics? A systematic review. J Community Genet. 2019;10:171–87. https://doi.org/10.1007/s12687-018-0394-0.
Google Scholar