Health professionals had suboptimal knowledge, positive attitudes, and suboptimal practices toward IBS. Their KAP can be influenced by gender, education, occupation, profession, sector, family with IBS, length of service, and type of educational institution. This study highlights the need for comprehensive strategies to increase knowledge, align attitudes with evidence-based practice, and overcome barriers to ultimately improve clinical practice and outcomes for patients with IBS. .
The results of this study on healthcare professionals' knowledge, attitudes, and practices regarding IBS indicate that there is a large gap between healthcare professionals' attitudes and knowledge, with relatively positive attitudes in contrast to poor knowledge scores. Shows 15. This discrepancy highlights the need for targeted educational interventions to close the knowledge and attitude gap16. Although these results are consistent with previous studies showing a lack of knowledge among healthcare professionals, it is still surprising that such a positive attitude does not consistently translate into optimal clinical practice. Addressing barriers such as time constraints and resource limitations is critical to improving patient care18.
Notably, knowledge scores showed variation based on gender, education, occupation, professional title, sector, and family members affected by IBS, and these factors clearly influence healthcare professionals' understanding of IBS19. It is suggested that Male participants had significantly higher knowledge than females, highlighting the importance of gender-specific educational interventions. Experts at higher education level, especially those with a master's degree or above, demonstrated greater depth of knowledge, highlighting the importance of higher education in increasing understanding20. Furthermore, differences in practice scores between different facility types suggest the potential influence of hospital setting on IBS management practices 21 . These findings highlight the need for customized strategies to address specific knowledge gaps, attitudes, and practices within different subgroups of health professionals22. To improve clinical practice and patient outcomes, targeted educational interventions, professional development programs, and institutional support systems are designed to comprehensively address these variations, thereby increasing the More effective and standardized care needs to be promoted23.
This study also revealed areas of agreement with established knowledge as well as critical gaps that require intensive discussion. Of note, this result supports several core findings in IBS, including the usefulness of colonoscopy to rule out organic lesions and the characteristic clinical symptoms of IBS, which are consistent with the general medical literature. Indicates that participants have a solid understanding of the concept24. This knowledge base is consistent with traditional diagnostic and epidemiological aspects of IBS and reflects proactive aspects of clinical practice. However, it is concerning that a significant proportion of participants were unfamiliar with complementary treatments such as acupuncture and traditional Chinese medicine's views on the pathogenesis of IBS. Furthermore, awareness of the potential association between infectious gastroenteritis and the development of irritable bowel syndrome is relatively limited, raising questions about the incorporation of new research findings into clinical practice. . To enhance clinical practice, targeted educational interventions are essential to promote a broader understanding of complementary therapies and ensure that health professionals are aware of evolving insights into the multifactorial nature of IBS. These interventions will fill existing knowledge gaps and enable healthcare professionals to provide more comprehensive, evidence-based care to patients with IBS25. The striking differences in perceptions regarding these alternative and emerging aspects of IBS may be due to differences in educational background, access to up-to-date information, or differences in institutional emphasis versus traditional approaches26. Therefore, it is essential to address these contradictions by integrating comprehensive and contemporary IBS education into health professional training programs and promoting continuous learning in clinical practice.
Respondent attitudes provide valuable insights that can greatly inform and improve clinical practice in the management of IBS. Medical professionals generally believe that the prognosis for IBS is good and emphasize the importance of patients maintaining a positive outlook, reflecting overall optimism within the medical community. Mas27. These positions highlight the potential benefits of adopting a patient-centered approach that not only addresses the physical aspects of IBS but also recognizes the importance of psychological health in symptom management. Furthermore, the strong consensus on the need to consider dietary habits and the role of patient involvement in achieving a good prognosis highlights the importance of comprehensive care that integrates dietary guidance and active patient participation. I am. Furthermore, the call for caution when considering differential diagnoses highlights the complexity of IBS diagnosis and the need for healthcare professionals to maintain a vigilant approach to rule out other conditions28. Furthermore, the recognition that health care professionals should play a vital role in educating patients to prevent IBS triggers emphasizes the importance of patient education and active preventive measures. Finally, the emphasis on the proficiency of non-gastroenterology health care professionals in recognizing symptoms of irritable bowel syndrome emphasizes the need for interdisciplinary collaboration and knowledge dissemination across specialties.
In terms of clinical practice, a significant proportion of healthcare professionals request IBS-related information and guidelines, reflecting a commitment to keeping their practice informed and evidence-based. This is consistent with the dynamic nature of medical knowledge and the need for continuous learning to provide optimal care29. Additionally, active participation in IBS-related training reflects a dedication to professional development and the importance of providing healthcare professionals with the latest insights and skills for IBS management. is emphasized. They play an important role in patient education and represent a comprehensive approach to IBS care. However, the potential for patients to skip necessary diagnostic tests due to misunderstandings suggests that communication and education with patients needs to be improved to protect them from important diagnostic procedures.
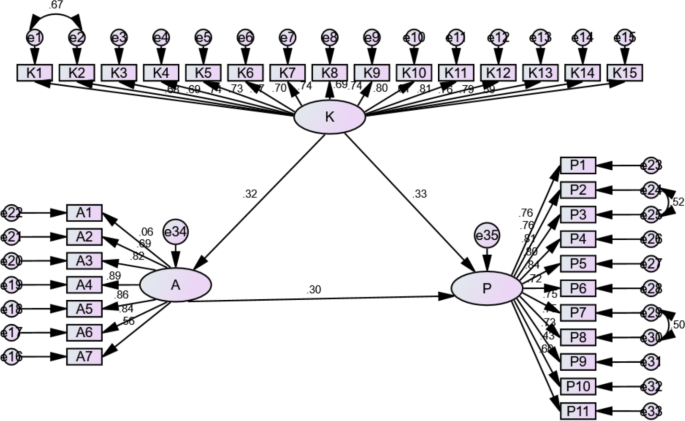
The results of the correlation analysis revealed significant associations between the main variables of this study. A positive correlation was observed between knowledge and attitudes 30 and between knowledge and practice, highlighting the interrelationship between these factors in the management of IBS among healthcare professionals. Furthermore, significant correlations were found between attitudes and practices, highlighting the unique relationship between these factors31. SEM analysis verified these relationships and showed a good model fit. Importantly, this analysis revealed a direct influence, with knowledge influencing both attitudes and practices, with attitudes playing a direct role in shaping practices. Collectively, these findings highlight the importance of strengthening knowledge as a basis for developing positive attitudes and translating it into clinical practice for more effective IBS management 32 .
This study had limitations. First, the cross-sectional design adopted in this study obtains data from a single time point, thus limiting the establishment of causal relationships between variables. This design limits the ability to ascertain whether changes in knowledge, attitudes, and practices occurred over time or were influenced by external factors. Additionally, this study was conducted in five hospitals in Shandong province within a specific time period, which may limit the generalizability of the study results to a broader range of healthcare workers in different settings across China. Additionally, the use of self-administered questionnaires may introduce response bias as participants may provide socially desirable answers or have different interpretations of survey items. Finally, a significant portion of the participants worked in gastroenterology, which may be biased by their specific professional background.